Diagnosis
Your health care provider will perform a physical exam and ask questions about your personal and family health history. You may be referred to a doctor that specializes in heart diseases (cardiologist).
Your provider may hear a whooshing sound (bruit) when listening to your arteries with a stethoscope.
Coronary calcium scan
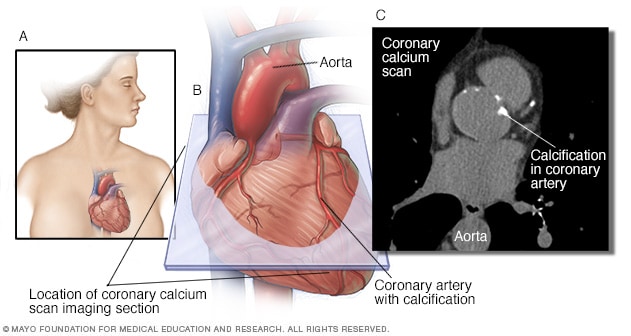
Coronary calcium scan
A coronary calcium scan uses computerized tomography (CT) imaging to take pictures of your heart's arteries. It can detect calcium deposits in the coronary arteries. Calcium deposits can narrow the arteries and increase the risk of a heart attack. The image on the left shows where the heart is typically located in the body (A). The middle image shows the area of the coronary calcium scan image (B). The image on the right shows a coronary calcium scan (C).
Depending on the results of the physical exam, your health care provider may suggest one or more tests, including:
- Blood tests. Blood tests are usually done to check blood sugar and cholesterol levels. High levels of blood sugar and cholesterol raise the risk of atherosclerosis. A C-reactive protein (CRP) test also may be done to check for a protein linked to inflammation of the arteries.
- Electrocardiogram (ECG or EKG). This quick and painless test measures the electrical activity of the heart. During an ECG, sensors (electrodes) are attached to the chest and sometimes to the arms or legs. Wires connect the sensors to a machine, which displays or prints the results. An ECG can help determine if there's reduced blood flow to the heart.
- Exercise stress test. If your symptoms usually occur during exercise, your health care provider may recommend this test. You'll walk on a treadmill or ride a stationary bike while your heart is monitored. Because exercise makes the heart pump harder and faster than it does during most daily activities, an exercise stress test can show heart problems that might otherwise be missed. If you can't exercise, you may be given a medication that mimics the effect of exercise on your heart.
- Echocardiogram. This test uses sound waves to show blood flow through the heart. Sometimes it is done with exercise stress testing.
- Doppler ultrasound. Your provider may use a special ultrasound device (Doppler ultrasound) to measure your blood pressure at various points along your arm or leg. These measurements can show the speed of blood flow in the arteries.
- Ankle-brachial index (ABI). This test compares the blood pressure in the ankle with that in the arm. It's done to check for atherosclerosis in the arteries in the legs and feet. A difference between the ankle and arm measurements may be due to peripheral vascular disease, which is usually caused by atherosclerosis.
- Cardiac catheterization and angiogram. This test can show if the coronary arteries are narrowed or blocked. A long, thin flexible tube (catheter) is inserted in a blood vessel, usually in the groin or wrist, and guided to the heart. Dye flows through the catheter to arteries in the heart. The dye helps the arteries show up more clearly on images taken during the test.
- Coronary calcium scan. Also called a heart scan, this test uses computerized tomography (CT) imaging to create detailed pictures of the heart. It can show calcium deposits in the artery walls. Results of the test are given as a score. When calcium is present, the higher the score, the higher the risk of heart disease.
- Other imaging tests. Magnetic resonance angiography (MRA) or positron emission tomography (PET) also may be used to study the arteries. These tests can show hardening and narrowing of large arteries, as well as aneurysms.
More Information
Treatment
Lifestyle changes, such as eating a healthy diet and exercising, may be all that is needed to treat atherosclerosis. But sometimes, medication or surgical procedures may be needed.
Medications
Many different drugs are available to slow — or even reverse — the effects of atherosclerosis. Here are some medications used to treat atherosclerosis:
-
Statins and other cholesterol drugs. Aggressively lowering low-density lipoprotein (LDL) cholesterol — the "bad" cholesterol — can slow, stop or even reverse the buildup of fatty deposits in the arteries.
Statins are commonly used to lower cholesterol, improve artery health and prevent atherosclerosis. There are many other types of cholesterol-lowering drugs. They include niacin, fibrates and bile acid sequestrants. You may need more than one type of cholesterol medication.
- Aspirin. Aspirin helps thin the blood and prevent blood clots. Daily low-dose aspirin therapy may be recommended for the primary prevention of heart attack or stroke in certain people. Daily use of aspirin can have serious side effects, including bleeding in the stomach and intestines. Don't start taking a daily aspirin without talking to your health care provider.
- Blood pressure medications. Drugs to lower blood pressure don't help reverse atherosclerosis. Instead they prevent or treat complications related to the disease. For example, certain blood pressure medications can help reduce the risk of a heart attack.
- Other medications. Drugs may be prescribed to control other health conditions — such as diabetes — that raise the risk of atherosclerosis. Medications may also be given to treat specific symptoms of atherosclerosis, such as leg pain during exercise.
Surgery or other procedures
Sometimes more aggressive treatment is needed to treat atherosclerosis. If you have severe symptoms or a blockage, you may need a procedure or surgery, including:
- Angioplasty and stent placement. This procedure — also called percutaneous coronary intervention (PCI) — helps open a clogged or blocked artery. A long, thin flexible tube (catheter) is inserted in a blood vessel, usually in the groin or wrist, and guided to the blockage. Then, a balloon on the tip of a catheter can be inflated to open the artery. A mesh tube (stent) is typically used to keep the artery open.
- Endarterectomy. Sometimes, surgery is needed to remove plaque from the walls of a narrowed artery. When the procedure is done on arteries in the neck (the carotid arteries), it's called a carotid endarterectomy.
- Fibrinolytic therapy. If a clot in an artery is blocking blood flow, your provider may use a clot-dissolving drug to break it apart.
- Coronary artery bypass graft (CABG) surgery. A surgeon takes a healthy blood vessel from another part of the body to create a new path for blood in the heart. The blood then goes around the blocked or narrowed coronary artery. CABG is an open-heart surgery. It's usually done only in those with many narrowed heart arteries.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Making certain lifestyle changes can help keep the arteries healthy and can prevent or slow atherosclerosis. Try these heart-healthy tips:
- Don't smoke. Smoking damages the arteries. Smoking is a major risk factor for coronary artery disease. Nicotine tightens blood vessels and forces the heart to work harder. Not smoking is one of the best ways to lower the risk of atherosclerosis complications, such as a heart attack.
-
Exercise most days of the week. Regular exercise improves blood flow, lowers blood pressure, and reduces the risk of conditions that increase the risk of atherosclerosis and heart disease.
Get at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous aerobic activity a week, or a combination of the two. You can take the stairs instead of the elevator, walk around the block during your lunch hour, or do some situps or pushups while watching television.
- Maintain a healthy weight. Being overweight increases the risk of coronary artery disease, which is caused by atherosclerosis. Losing even a small amount of weight can help reduce the risk.
-
Eat healthy foods. A heart-healthy diet full of fruits, vegetables and whole grains — and low in refined carbohydrates, sugars, saturated fat and sodium — can help control weight, blood pressure, cholesterol and blood sugar.
Try substituting whole-grain bread in place of white bread. Grab an apple, a banana or carrot sticks as a snack. Read nutrition labels to check the amount of salt and fat. Use monounsaturated fats, such as olive oil. Reduce or avoid sugar and sugar substitutes.
- Manage stress. Find ways to help reduce emotional stress. Getting more exercise, practicing mindfulness and connecting with others in support groups are some ways to tame stress. Relaxation techniques, such as yoga or deep breathing, also may be helpful. These practices can temporarily lower blood pressure, reducing the risk of developing atherosclerosis.
If you have high cholesterol, high blood pressure, diabetes or another chronic disease, work with your health care provider to manage the condition and promote overall health.
Alternative medicine
It's thought that some foods and herbal supplements may help reduce high cholesterol and high blood pressure, two major risk factors for developing atherosclerosis. Alternative medicine supplements and products that may be effective for atherosclerosis include:
- Alpha-linolenic acid
- Barley
- Beta-sitosterol (found in supplements and some margarines, such as Promise Activ)
- Blond psyllium (found in seed husk and products such as Metamucil)
- Calcium
- Cocoa
- Fish oil
- Garlic
- Green tea
- Oat bran (found in oatmeal and whole oats)
- Sitostanol (found in supplements and some margarines, such as Benecol)
Talk to your health care provider before adding any of these or other supplements to your atherosclerosis treatment. Some supplements can interact with medications, causing harmful side effects.
Preparing for your appointment
If you think you may have atherosclerosis or are concerned about having atherosclerosis because of a strong family history of heart disease, make an appointment with your provider to have your cholesterol level checked.
Here's some information to help you get ready for your appointment.
What you can do
- Be aware of any pre-appointment restrictions. When you make the appointment, ask whether there's anything you need to do in advance, such as restrict your diet. Many blood tests, including cholesterol and triglycerides, require that you avoid eating and drinking for a certain number of hours before the tests.
- Write down any symptoms you're having. Atherosclerosis is a risk factor for heart disease. Always tell your provider if you have symptoms such as chest pains or shortness of breath. Such information helps guide treatment.
- Write down important personal information, including a family history of high cholesterol, heart disease, stroke, high blood pressure or diabetes, and any major stresses or recent life changes.
- Make a list of all medications, vitamins or supplements you're taking. Include dosages.
- Take a family member or friend along, if possible. Someone who goes with you may remember something that you missed or forgot.
- Be prepared to talk about your diet and exercise habits. If you don't already eat a healthy diet or exercise, your provider can give you tips on how to get started.
- Write down questions to ask your health care provider.
Preparing a list of questions will help you make the most of your time with your health care provider. For atherosclerosis, some basic questions to ask your provider include:
- What tests will I need?
- What's the best treatment?
- What foods should I eat or avoid?
- What's an appropriate level of exercise?
- How often do I need a cholesterol test?
- What are the options to the primary treatment you're suggesting?
- Is there a generic alternative to the medicine you're prescribing?
- I have other health conditions. How can I best manage them together?
- Should I see a specialist?
- Are there brochures or other printed material that I can take with me? What websites do you recommend?
Don't hesitate to ask any other questions you have.
What to expect from your doctor
Your health care provider is likely to ask many questions, including:
- Do you have a family history of high cholesterol, high blood pressure or heart disease?
- What are your diet and exercise habits like?
- Do you or did you smoke or use tobacco in any form?
- Do you have discomfort in your chest or pain in your legs with walking or at rest?
- Have you had a stroke or unexplained numbness, tingling or weakness of one side of your body, or difficulty speaking?
What you can do in the meantime
It's never too early to make healthy lifestyle changes, such as quitting smoking, eating healthy foods and getting more exercise. These are simple ways to protect yourself against atherosclerosis and its complications, including heart attack and stroke.