Overview
Angina (an-JIE-nuh or AN-juh-nuh) is a type of chest pain caused by reduced blood flow to the heart. Angina is a symptom of coronary artery disease.
Angina also is called angina pectoris.
Angina is often described as squeezing, pressure, heaviness, tightness or pain in the chest. It may feel like a heavy weight lying on the chest. Angina may be a new pain that needs to be checked by a healthcare professional, or it may be recurring pain that goes away with treatment.
Angina is relatively common. But some people may not be able to tell it apart from other types of chest pain, such as heartburn. If you have unexplained chest pain, get medical help right away.
Types
There are different types of angina. The type depends on the cause and whether rest or medicine eases symptoms.
-
Stable angina. Stable angina is the most common form of angina. It usually happens during activity, also called exertion. It goes away with rest or angina medicine. Pain that starts when you're walking uphill or in the cold weather may be angina.
Stable angina is predictable. It is usually similar to previous episodes of chest pain. The chest pain typically lasts a short time, perhaps five minutes or less.
- Unstable angina, which is a medical emergency. Unstable angina is unpredictable and occurs at rest. Or the pain is worsening and occurs with less physical effort. Unstable angina is typically severe and lasts longer than stable angina, maybe 20 minutes or longer. The pain doesn't go away with rest or the usual angina medicines. If the blood flow doesn't improve, the heart doesn't get enough oxygen. A heart attack occurs. Unstable angina is dangerous and needs emergency treatment.
- Variant angina, also called Prinzmetal angina. This type of angina isn't due to coronary artery disease. It's caused by a spasm in the heart's arteries. The spasm temporarily reduces blood flow. Severe chest pain is the main symptom of variant angina. It most often occurs in cycles, typically at rest and overnight. The pain may be relieved by angina medicine.
- Refractory angina. Angina episodes are frequent despite a combination of medicines and lifestyle changes.
Symptoms
Heart attack
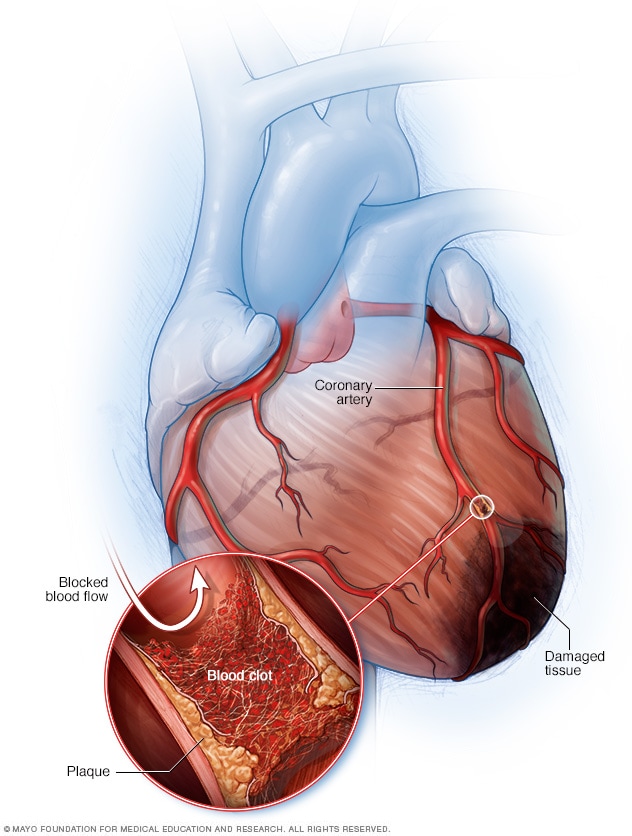
Heart attack
A heart attack occurs when an artery supplying the heart with blood and oxygen becomes blocked. Fatty deposits build up over time, forming plaques in the heart's arteries. If a plaque ruptures, a blood clot can form and block the arteries, causing a heart attack. During a heart attack, tissue in the heart muscle dies due to lack of blood flow through the heart's arteries.
Angina symptoms include chest pain and discomfort. The chest pain or discomfort may feel like:
- Burning.
- Fullness.
- Pressure.
- Squeezing.
Pain also may be felt in the arms, neck, jaw, shoulder or back.
Other symptoms of angina include:
- Dizziness.
- Fatigue.
- Nausea.
- Shortness of breath.
- Sweating.
The severity, duration and type of angina can vary. New or different symptoms may signal unstable angina or a heart attack.
Any new or worsening angina symptoms need to be checked immediately by a healthcare professional. The healthcare team can determine whether you have stable or unstable angina.
Angina in women
Symptoms of angina in women can be different from the classic angina symptoms. These differences may lead to delays in seeking treatment. For example, chest pain may not be the only symptom or the most common symptom. Other symptoms of angina in women may include:
- Discomfort in the neck, jaw, teeth or back.
- Nausea.
- Shortness of breath.
- Stabbing pain instead of chest pressure.
- Stomach pain.
When to see a doctor
Chest pain that lasts longer than a few minutes and doesn't go away with rest or angina medicines may be due to a heart attack. Call 911 or emergency medical help. Only drive yourself to the hospital if there is no other way to get there.
If chest discomfort is a new symptom for you, see a healthcare professional to determine the cause and to get proper treatment. If you have stable angina and it gets worse or changes, seek medical help immediately.
Causes
Angina is caused by reduced blood flow to the heart muscle. Blood carries oxygen, which the heart muscle needs to survive. When the heart muscle isn't getting enough oxygen, it causes a condition called ischemia.
The most common cause of reduced blood flow to the heart muscle is coronary artery disease (CAD). The heart arteries, called the coronary arteries, can become narrowed by fatty deposits called plaques. This condition is called atherosclerosis.
Plaque in a blood vessel may rupture or cause a blood clot. These events can quickly block or reduce flow through a narrowed artery. This can suddenly and severely decrease blood flow to the heart muscle.
The heart muscle may still be able to work during times of low oxygen demand without triggering angina symptoms. An example is when resting. But when the demand for oxygen goes up, such as when exercising, angina can result.
Risk factors
The following things may increase the risk of angina:
- Increasing age. Angina is most common in adults age 60 and older.
- Family history of heart disease. Tell your healthcare team if your mother, father or any siblings have or had heart disease or a heart attack.
- Tobacco use. Smoking, chewing tobacco and long-term exposure to secondhand smoke can damage the lining of the arteries. Artery damage can let deposits of cholesterol collect and block blood flow.
- Diabetes. Diabetes increases the risk of coronary artery disease. Coronary artery disease can cause angina.
- High blood pressure. Over time, high blood pressure damages arteries by speeding up the hardening of the arteries.
- High cholesterol or triglycerides. Too much bad cholesterol, called low-density lipoprotein (LDL), in the blood can cause arteries to narrow. A high LDL level increases the risk of angina and heart attack. A high level of triglycerides in the blood also is unhealthy.
- Other health conditions. Chronic kidney disease, peripheral artery disease, metabolic syndrome or a history of stroke increases the risk of angina.
- Not enough exercise. An inactive lifestyle raises the risk of high cholesterol, high blood pressure, type 2 diabetes and obesity. Talk with your healthcare team about the type and amount of exercise that's best for you.
- Obesity. Obesity is a risk factor for heart disease, which can cause angina. Being overweight makes the heart work harder to supply blood to the body.
- Emotional stress. Too much stress and anger can raise blood pressure. Rushes of hormones made by the body during stress can narrow the arteries and worsen angina.
- Medicines. Some medicines tighten blood vessels, which may trigger Prinzmetal angina. An example is certain migraine medicines.
- Drug misuse. Cocaine and other stimulants can cause blood vessel spasms and trigger angina.
- Cold temperatures. Exposure to cold temperatures can trigger Prinzmetal angina.
Complications
The chest pain that occurs with angina can make doing some activities, such as walking, uncomfortable. However, the most dangerous complication is a heart attack.
Warning symptoms of a heart attack include:
- Pressure, fullness or a squeezing pain in the center of the chest that lasts for more than a few minutes.
- Pain extending beyond the chest to the shoulder, arm or back, or even to the teeth and jaw.
- Fainting.
- Threatening sense of doom.
- Increasing episodes of chest pain.
- Nausea and vomiting.
- Continued pain in the upper belly area.
- Shortness of breath.
- Sweating.
If you have any of these symptoms, seek emergency medical attention immediately.
Prevention
You can help prevent angina by following the same lifestyle changes that are used to treat angina:
- Avoid or limit alcohol.
- Don't smoke.
- Eat a healthy diet.
- Exercise regularly.
- Maintain a healthy weight.
- Manage other health conditions related to heart disease.
- Reduce stress.
- Get 7 to 9 hours of sleep a day.
Also get recommended vaccines to avoid heart complications.