June 10, 2022
腰椎管狭窄症
腰椎管狭窄症
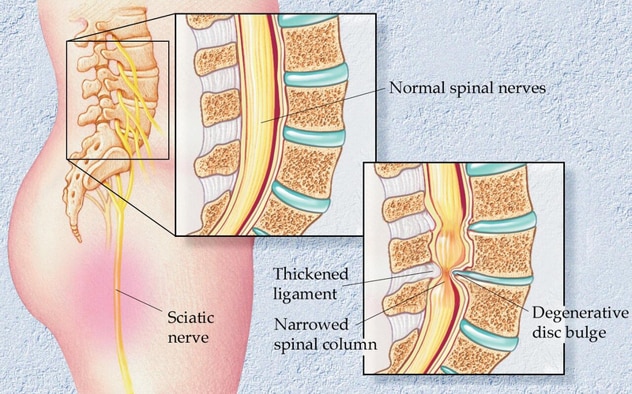
腰椎管狭窄症是指椎管狭窄,通常由椎间盘退变或突出、椎体半脱位、小关节增生或韧带增厚所致。
Lumbar spinal stenosis (LSS) is a narrowing of the spinal canal that often occurs as a result of disk degeneration or herniation, subluxation of the vertebrae, overgrowth of the facets, or thickening of the ligaments. Additional, less common causes of narrowing include tumor, infection, fracture and epidural lipomatosis.
Symptoms
LSS seen on imaging can be asymptomatic. However, it can lead to chronic pain, disability and decreased quality of life. Women age 70 and older are the population most affected by LSS. In people over age 65, LSS is one of the most common reasons for surgery.
Symptomatic LSS typically starts gradually. As the spinal canal narrows, it can compress the nerve roots, causing pseudoclaudication. This compression can result in pain, heaviness, weakness, or paresthesia in the buttocks, legs and feet during walking or prolonged standing.
Pain caused by pseudoclaudication is typically relieved by sitting or by bending forward at the waist to reduce pressure on the affected nerves. In individuals with advanced stenosis, sitting or lying down may no longer provide symptom relief.
Medical management
Management options for LSS include watchful waiting, physical therapy, equipment and modalities, medications, injections, and surgical referral. According to Kimberly (Kim) L. Seidel-Miller, M.D., a physiatrist at Mayo Clinic's Spine Center in Rochester, Minnesota, there are several issues to consider that can help guide the medical management of LSS.
"It's important to assess the patient's severity of symptoms and level of disability," explains Dr. Seidel-Miller. "This assessment should include documenting the patient's pain level and identifying the degree to which LSS may affect various aspects of their life, including mobility, mood, and ability to participate in activities of daily living, work, hobbies or interest." Symptom longevity and progression as well as response to any past interventions, including physical therapy, medications or injections, can also help determine next steps.
-
Watchful waiting
According to Dr. Seidel-Miller, watchful waiting may be appropriate for several types of patients with LSS. "This would include individuals with asymptomatic stenosis, individuals with mild or primarily axial symptoms, or individuals who prefer to wait before trying interventions."
-
Physical therapy, equipment and modalities
Weight loss and physical therapy are common first line treatments recommended for reducing lumbar lordosis. "Physical therapy can introduce patients to a mix of exercises and movements that help correct posture, address radicular symptoms, stretch the low back and lower limbs, and strengthen the supporting core and trunk musculature," says Dr. Seidel-Miller. "Lumbosacral corsets and gait aids can also be used to reduce lumbar lordosis and improve mobility. Other modalities, such as transcutaneous electrical nerve stimulation, ultrasound, heat or cold therapy, and traction, can also be effective."
-
Medications
The list of medications commonly used to treat LSS symptoms includes topical agents such as lidocaine, menthol, camphor and capsaicin, over-the-counter analgesics and anti-inflammatories, and neuropathic agents such as gabapentin and pregabalin. These medications are typically more beneficial for those with radicular symptoms as opposed to pseudoclaudication.
-
Injections
Intralaminar epidural injections can be used to treat symptoms related to neurogenic claudication. Patients with radicular symptoms often experience better symptom relief with transforaminal epidural injections. Effectiveness and longevity of benefit from these injections can vary depending on the cause and severity of the LSS.
In an article published in Pain Practice in 2020, Dr. Jang and co-investigators followed 54 patients who were treated with transforaminal epidural steroid injections for lumbar radicular pain from spinal stenosis. At a 5-to-7-year follow-up, only about 15% of the patients reported complete resolution of the initial pain, while about 50% of the patients had significant pain and required additional injections every 2 to 6 months or oral medications.
-
Surgical referral
Surgical referral should be considered when patients have persistent or progressive weakness or numbness, or changes in bowel or bladder function, or when significant symptoms persist despite the above medical management interventions.
Future treatment options
Dr. Seidel-Miller is hopeful that future research will yield improved data on patient outcomes associated with radicular versus claudicatory symptoms, to better guide clinicians in selecting appropriate treatment approaches. "Research focused on personalized medicine and regenerative medicine approaches could offer more-effective treatment options for LSS," notes Dr. Seidel-Miller. "Results of research exploring the use of stem cell therapies for degenerative disk disease and the search for genetic markers for spinal degeneration could facilitate early diagnosis and help identify patients who might benefit from these new therapeutic approaches."
For more information
Jang SH, et al. At least 5-year follow-up after transforaminal epidural steroid injection due to lumbar radicular pain caused by spinal stenosis. Pain Practice. 2020;20:748.
Refer a patient to Mayo Clinic.