Sept. 24, 2019
Mayo Clinic has the breadth of expertise to individualize treatment of proximal humeral fractures. With experience in the full range of treatment modalities, Mayo's orthopedic surgeons are able to provide a treatment approach — sling, repair or replacement — based on the needs of each patient.
"Our No. 1 goal is figuring out who needs an operation, and which operation. We have all options available to us at all times," says Jonathan D. Barlow, M.D., an orthopedic surgeon at Mayo Clinic in Rochester, Minnesota.
The management of proximal humeral fractures has evolved rapidly, allowing for improved patient treatment. However, decisions about managing care are sometimes based on a surgeon's background, with trauma-trained orthopedic surgeons opting for repair and shoulder surgeons choosing reverse total shoulder replacement.
肱骨近端骨折治疗前和治疗后
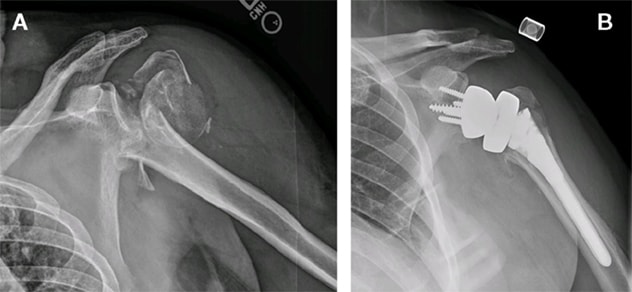
肱骨近端骨折治疗前和治疗后
A. 一名 62 岁男士的 X 线检查显示他跌倒后发生了肱骨近端骨折。在与患者仔细讨论治疗方案后,该患者接受了反向全肩关节置换术。B. 术后 6 周的 X 线检查显示结节已基本实现解剖学愈合。
"Mayo is bridging this gap, to optimize surgical management of these fractures," Dr. Barlow says. "We know from our research and our experience treating patients that certain people are better off with reverse total shoulder repair, while others can be reliably treated with proximal humeral fracture plates."
With training in both trauma and shoulder orthopedics, Dr. Barlow is part of an orthopedics team with multimodal expertise. "Mayo Clinic has always been at the forefront of new and different modalities. We've established our expertise with reverse total shoulder repair and also evolved the mechanics of how plate fixation is applied, to substantially lower complication rates," he says.
The right surgery at the right time
Mayo's approach to these fractures depends on such factors as the patient's age, bone quality and source of injury. Patients younger than 60 to 65 are often candidates for surgical repair. "They tend to have good bone and to have experienced high-energy trauma from motor vehicle accidents or falls from heights. We have shown that we can successfully treat those patients with plates and screws," Dr. Barlow says.
Patients older than 65 or with lower bone quality are less likely to have good outcomes from surgical repair and typically have shoulder replacement. "We have a robust shoulder arthroplasty division," Dr. Barlow says. "Our outcomes have been reliably good, with most patients regaining overhead motion, and complication rates of around 5% — which is quite low for such a bad fracture."
Proximal humeral fractures are especially debilitating for older patients, who often rely on their upper extremities to ambulate and to push themselves out of chairs. Surgical treatment is sometimes avoided with the assumption that it remains an option if nonsurgical treatment fails.
"But functional outcomes are lower if a patient is initially treated without surgery and then has a shoulder replacement later," Dr. Barlow says. "If we don't make the right decision the first time, we're subjecting older patients to repetitive surgeries with the potential for morbidity and the need for hospitalization and use of skilled nursing facilities."
To learn more about optimal treatment approaches for proximal humeral fractures, Mayo Clinic is planning a randomized trial comparing nonsurgical treatment to reverse total shoulder replacement. A 2015 trial in the U.K., published in JAMA in 2015, found no significant difference in outcomes between patients who had surgical repair and nonsurgical treatment for these fractures. The U.K. study, which had a two-year follow-up period, didn't investigate reverse total shoulder replacement.
"We think this area warrants further investigation using modern shoulder replacement techniques," Dr. Barlow says. "There's tremendous uncertainty among many physicians about the optimal approach for an individual patient. Mayo Clinic is committed to individualized treatment."
For more information
Rangan A, et al. Surgical vs nonsurgical treatment of adults with displaced fractures of the proximal humerus: The PROFHER randomized clinical trial. JAMA. 2015;313:1037.