Dec. 20, 2022
骨量丢失
骨量丢失
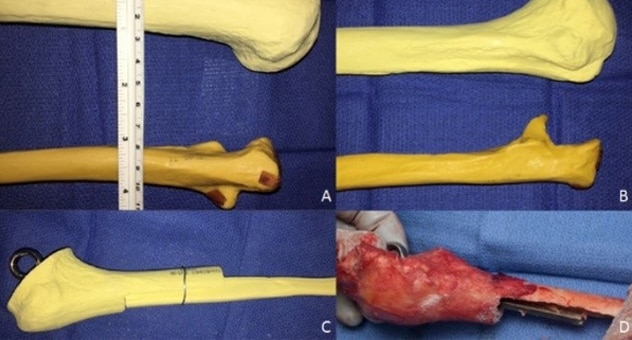
这些图像显示需要 TEA 翻修的患者存在大量骨量丢失。
Mark E. Morrey, M.D., an orthopedic surgeon specializing in elbow and shoulder repair at Mayo Clinic in Rochester, Minnesota, enjoys a challenge. In fact, the idea of solving complicated elbow problems drew him into research and practice in this area. A key question that emerged for him was how to effectively and safely help patients whose total elbow arthroplasties (TEAs) have failed. These patients develop complex skeletal defects with significant bone loss due to tumors, infection or trauma. While symptoms are effectively treated following the primary elbow replacement, if the implant loosens, it can lead to massive bone deficiency.
"I chose to pursue elbow replacements, especially revisions, because it's challenging," he says. "Many times, we represent the last line to save the elbow. Unlike hip and knee repair, there have not been great options for patients with massive bone loss at the elbow joint. This was a clinical void; we needed solutions."
Dr. Morrey's father, Bernard F. Morrey, M.D., former chair of Orthopedic Surgery at the same Mayo Clinic campus, also pursued elbow reconstruction clinical research. He has performed thousands of TEAs and revisions.
"I'm standing on the shoulders of giants," says Dr. Mark Morrey, referring to his father and other Mayo Clinic elbow surgeons who came before him. "I'm proceeding in what I learned from my mentors."
At Mayo Clinic, Dr. Bernard Morrey performed revision TEA allograft-prosthetic composites for patients with failed previous TEAs. He joined an allograft to the patient's remaining bone and added a prosthesis. Yet, Dr. Mark Morrey explains, allograft-prosthetic composites had high complication rates, often plagued by issues such as infection or nonunion. Although this revision procedure appeared promising compared with previously utilized megaprostheses, complications prompted Dr. Bernard Morrey to put a moratorium on this procedure. He directed the revision TEA group to use other methods instead. Unfortunately for some defects, bone struts did not fill all the elbow joint space and conditions associated with bone loss continued to increase.
'Patients kept coming'
Complication rates for revision TEA with allograft-prosthetic composite did not slow reconstructive demand, however. Therefore, Dr. Mark Morrey and colleagues continued to pursue options to help patients with these challenging reconstructive problems.
"There was no good solution for patients with failed TEAs and massive bone loss, but patients kept coming," says Dr. Morrey. "We needed a reliable salvage for these patient's elbows. Even if difficult, that doesn't mean we don't do it or try it."
Although patients requiring revision TEA had been mostly older adults, Dr. Mark Morrey says younger patient demand grew due to substantial post-traumatic arthritis-related elbow joint bone loss. As these patients are typically working age and need their livelihoods, a nonfunctional elbow was unacceptable if the initial TEA failed. Thus, Dr. Morrey and team became even more determined to develop solutions for these revisions.
"A young person who's been in a car crash has higher elbow functional demands," he explains. "They've lost function; their quality of life is drastically diminished," says Dr. Morrey. "They have a completely dysfunctional arm, having lost so much joint surface, they can't flex or extend their elbows. Sometimes, they've lost so much bone the arm feels floppy and unstable. Pain awakening them from sleep, stiffness and dysfunction must also be addressed. You need good motor skills for many jobs. If the joint is fused or floppy, you can't position your hand in space."
Similar solution, new methodology
Mayo Clinic TEA revision specialists realized they needed to refine their techniques. They especially desired to prevent infection — plaguing 30% of patients after revision surgery, surpassing primary TEA, according to a 2006 Journal of Bone and Joint Surgery article — and improve elbow function.
Post-TEA infection results in significant bone loss. In the elbow joint, addressing infection was difficult in a revision due to nearby nerves and the volume of bone loss.
TEA 步骤
TEA 步骤
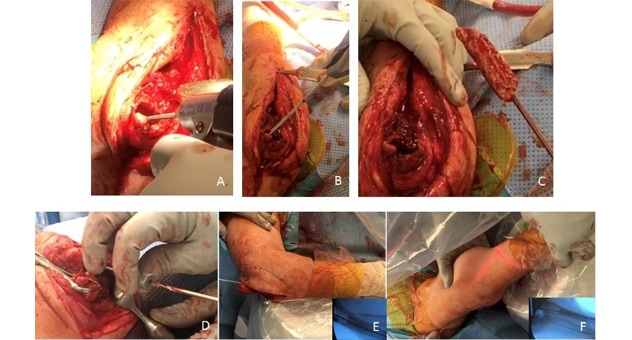
这些图像显示了 TEA 翻修中完成的步骤。
Dr. Mark Morrey felt high complication rates with revision TEA could be overcome. He also thought allograft-prosthetic composites remained the strongest option for patients with failed TEA, but with adaptation to new procedures. Dr. Morrey and colleagues developed a new TEA revision protocol to treat infection first, then perform an allograft prosthetic reconstruction.
清除骨水泥
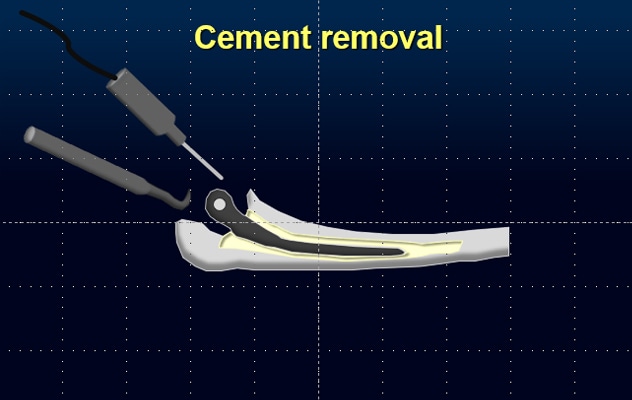
清除骨水泥
在 TEA 翻修过程中,外科医生通常需要清除既往 TEA 中使用的所有骨水泥。
They recognized a need for the following in revision TEA:
- Efficiency. As infection risk increases with surgical time, they had to perform successful revisions in shorter time to lessen infection risk.
- Pre-work. They decided to use advanced imaging studies to improve their understanding of the anatomy and better plan for the bone grafts that would be needed.
- 3D printing. They began using 3D-printed guides fitting the patient's defect.
- Complete cement removal. They started to remove all of the cement from previous TEAs. They had discovered failure to remove all of the cement increases infection rates.
- Customization. They began customizing each revision TEA to the patient to optimize the bone interface, improving the chances of bone union.
The result of this work is that the team has improved complication rates, including nonunion and infection.
"We're about 7 out of 10 in successful revisions of these TEAs now," he says. "We can restore function and cure infection in many cases, plus improve skeletal support for the implants. We've also made the surgery more reproducible."
Dr. Morrey indicates he and two Mayo Clinic colleagues performing the majority of TEA revisions formed an entire system around this surgery. Now, through improved revision TEA, they can increase elbow function. For example, if the elbow Mayo Elbow Performance Score was in the 60s, they can increase it to the 80s. In fact, a publication in The Journal of Bone and Joint Surgery indicates mean Mayo Elbow Performance Score for 25 patients increased from 30 to 84 at follow-up for revision TEA with allograft-prosthetic composites, 92% of which incorporated.
Patient case: Resigned to amputation
Dr. Mark Morrey explains one of his patients thrived for 15 years post-TEA, then developed a surgical site infection. The patient had eight operations, all failures.
When he went to see Dr. Morrey the patient said, "I know I need an amputation."
Nonetheless, Dr. Morrey thought he could help this patient with successful TEA revision. The patient decided to proceed. In the revision surgery, Dr. Morrey noted significant cement remaining in the joint.
"If I see retained cement, I worry debridement was insufficient in the previous surgeries," says Dr. Morrey. "I know any dead tissue or cement left behind can harbor infection."
Dr. Morrey recounts the patient had 10 centimeters of bone loss at the end of his humerus and only half of the ulna remained, which he calls "not a great place to start."
The patient's surgery included thorough cement removal, debridement and remnant bone cleaning. Dr. Morrey then linked and pinned the joint, using antibiotic cement. Making a flat cut across the humerus, he eyed the graft guide overlap, placing the elbow replacement through the allograft. He says he is grateful for the guides to prepare perfect surfaces, improving healing and rotational control, and avoiding loosening. He then used an additional triceps attachment allograft to restore power to the elbow.
术后 2 个月

术后 2 个月
一名患者在 TEA 翻修术后 2 个月的肘部情况。
Three months postoperatively, the patient's hand and elbow were functional. As the patient thought he was facing amputation before meeting Dr. Morrey, he was enormously grateful, seeing his results. He is now two years after his reconstructive surgery and extremely pleased with his results.
Surgical referrals and physician education
Dr. Mark Morrey and his colleagues welcome revision TEA referrals from physicians.
He says Mayo Clinic has one of the largest TEA volumes worldwide and correspondingly has the highest revision burden. Dr. Morrey indicates most trained shoulder and elbow surgeons perform 8 to 10 TEAs yearly. He has performed approximately 40 allograft-composite surgeries in the past year.
Dr. Morrey also indicates he and colleagues desire to teach others what they have learned and view imparting knowledge as an integral part of their roles. They are available for video calls with surgeons and their patients unable to travel or for video consults with the surgeon alone.
"We want good results whether the patient comes to Mayo or not," he says. "These are challenging problems, but there are salvage options that can give patients back their lives."
For more information
Parvizi J, et al. Periprosthetic infections: What are the diagnostic challenges? The Journal of Bone & Joint Surgery. 2006;88-A(suppl 4):138.
Cheng H, et al. Prolonged operative duration increases risk of surgical site infections: A systematic review. Surgical Infections. 2017;18:722.
Morrey ME, et al. Allograft-prosthetic composite reconstruction for massive bone loss including catastrophic failure in total elbow arthroplasty. The Journal of Bone & Joint Surgery. 2013;95:1117.
Refer a patient to Mayo Clinic.