Nov. 01, 2019
Mayo Clinic continuously evaluates its use of quantifiable CT perfusion imaging in acute ischemic stroke, fine-tuning the approach to optimize patient outcomes. The adjustments, which build on recent advances in stroke imaging technology, are implemented enterprisewide for consistent patient care.
"We are in a period of very rapid change in the evolution of stroke imaging," says E. Paul Lindell, M.D., a neuroradiologist at Mayo Clinic in Rochester, Minnesota. "This dynamic environment requires continuous monitoring of developments and of clinical cases to determine the best care for patients."
The DAWN and DEFUSE 3 clinical trials demonstrated that quantifiable CT perfusion can widen the treatment window for acute ischemic stroke. "There is now strong evidence to support the adoption of mechanical thrombectomy all the way up to 24 hours after stroke onset. But patients in this extended time window need to be carefully selected," says Bart M. Demaerschalk, M.D., a stroke neurologist at Mayo Clinic in Phoenix/Scottsdale, Arizona, and enterprise chair of cerebrovascular neurology. "We're committed to compiling what we collectively learn across our enterprise to better stratify patients for treatment."
出现急性缺血性脑卒中体征的一名女性的 CT 成像
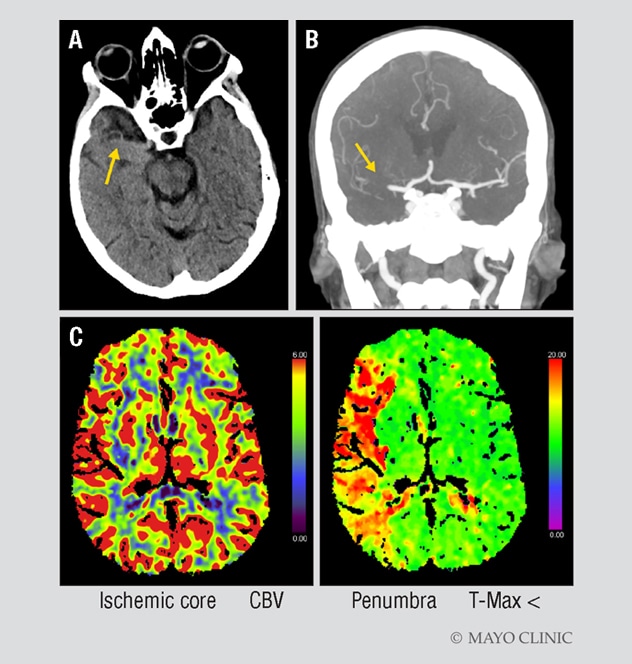
出现急性缺血性脑卒中体征的一名女性的 CT 成像
A. 一名 70 岁女性的 CT 显示存在大脑高密度征(箭头处)和右侧视物偏好,无出血。这名女性因急性左面部下垂、左臂无力和言语不清而来到妙佑医疗国际佛罗里达州杰克逊维尔院区就诊。她的初始 NIH 卒中量表评分为 17 分;Alberta 卒中项目早期 CT 评分(ASPECTS)为 10 分。B. CT 血管造影片证实存在大脑右中动脉血栓(箭头处)。C. CT 灌注成像显示缺血核心区(左图红色区域)和半暗带(右图绿色区域)之间存在较大的不匹配。
手术移除血块后的血管造影
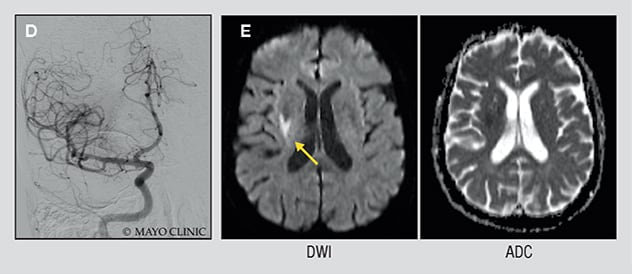
手术移除血块后的血管造影
D. 手术移除血块后的血管造影显示血流正常。E. 初始表现后两天的弥散加权成像(左)和表观扩散系数映射(右)显示患者的卒中非常小。她没有出现临床缺陷。
Mayo Clinic's considered use of perfusion CT provides an individualized approach to acute ischemic stroke. "Instead of treating every patient the same, we're making sure we use this technology appropriately to identify patients who can benefit from endovascular treatment," says James P. Klaas, M.D., a stroke neurologist at Mayo Clinic's campus in Minnesota. "There's no question that time is brain. But not every brain's time is the same."
Unique perspective
Mayo Clinic has stroke neurologists not only at its three main campuses in Arizona, Florida and Minnesota but also within Mayo Clinic Health System and at satellite sites via Mayo's telestroke network. This expertise, coupled with the high volume of patients treated for acute ischemic stroke, is advancing the application of CT perfusion to patient care.
"When a clinical trial is transformative, the results must still be translated into daily practice," Dr. Klaas says. "Our learning about CT perfusion is based on individual patient cases where certain aspects didn't precisely match up with the clinical trials. We don't want to miss a treatment option for a patient, but we also want to avoid treatment that would expose a patient to risk."
Mayo Clinic's refinements to CT perfusion rest on close collaboration among stroke neurologists, neurosurgeons, neurointerventionalists, neuroanesthesiologists and neuroradiologists. "We have a unique perspective, as an academic medical center and a health system, that informs our discussions," Dr. Lindell says. "Our multidisciplinary approach allows us to improve upon the results of clinical trials as we put them into practice."
Disseminating that knowledge enterprisewide benefits individuals in geographic areas where the risk of acute ischemic stroke is high. Through the telestroke network, Mayo Clinic stroke neurologists manage care in more than 30 hospitals in seven states as well as in telemedicine-enabled ambulances en route to hospitals.
"Our telestroke capability brings our expertise to communities that don't have subspecialized stroke neurologists," says Michelle P. Lin, M.D., M.P.H., a stroke neurologist at Mayo Clinic in Jacksonville, Florida. "The telemedicine assessment can select the patients most likely to benefit from thrombectomy. If a center doesn't have CT perfusion imaging, we can transfer patients promptly to a main campus."
Overall, the volumetric precision offered by quantifiable CT perfusion is benefitting patient care. Traditionally, patients who presented six hours after the onset of acute ischemic stroke were simply monitored. "The best we could do was try to manage the medical complications that arise with a large stroke," Dr. Demaerschalk says. "Now the expanded therapeutic window is translating into carefully selected patients having visible improvement in the first 24 to 72 hours after treatment. These patients are able to undergo rehabilitation and to stand, walk, talk and go home. It's quite striking."
In an era of rapid technological advancement, refining the application of this technology will remain key. "Right now, CT perfusion software treats every milliliter of brain the same. But we know that some areas are more critical for predicting neurological dysfunction," Dr. Klaas says. "One question is whether we should weight those areas differently."
Another potential development is a role for artificial intelligence in CT perfusion. "We think that artificial intelligence may be able to discriminate features that humans aren't able to discern in the images," Dr. Lindell says. "The images that we acquire probably aren't going to change a lot — it's the analysis that's so in flux."