March 26, 2022
As a level 4 comprehensive epilepsy center, Mayo Clinic is at the forefront of managing pediatric seizure conditions. A key component is identifying the etiology of an individual's seizures and beginning innovative therapies as early in life as possible.
"We are increasingly seeing specific therapies that target the underlying causes of pediatric epilepsy," says Elaine C. Wirrell, M.D., a pediatric epileptologist at Mayo Clinic Children's Center in Rochester, Minnesota. "These therapies hold potential to improve a child's development, provided we intervene early enough with the most effective treatment."
Dr. Wirrell co-chairs an International League Against Epilepsy task force that released a set of draft papers defining various epilepsy syndromes. "Our effort is driven partly by the emergence of newly licensed syndrome-specific medications, including gene-related therapies," she says.
Precisión de sitios donde se originan las convulsiones
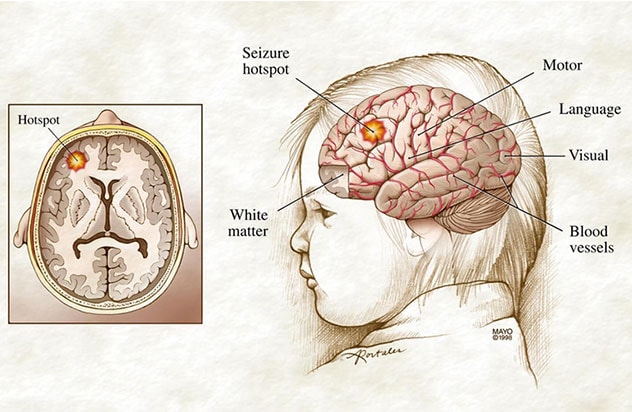
Precisión de sitios donde se originan las convulsiones
Las vistas laterales y transversales del cerebro de un niño muestran las principales áreas de funciones cerebrales y un punto de alta actividad que podría extirparse quirúrgicamente para prevenir convulsiones en el futuro.
For children with medication-resistant epilepsy, Mayo Clinic Children's Center offers a range of surgical treatments. These may involve surgical resection or laser ablation of a brain area where the seizures start. Neurostimulation — with implanted or noninvasive devices that aren't commonly used to treat pediatric epilepsy — is also an option at Mayo Clinic.
Level 4 is the highest rating designated by the National Association of Epilepsy Centers. In addition to providing extensive medical and surgical treatments, a level 4 center offers sophisticated neurodiagnostic monitoring and neuropsychological and psychosocial therapies.
"We recommend individualized treatments that are tailored to the child," says Donnie (Keith) K. Starnes II, M.D., a neurologist at Mayo Clinic Children's Center in Minnesota. "No two children with epilepsy are the same. We're not limited in terms of the available approaches, and we spend a lot of time talking to families about their options."
Advanced evaluation and surgical techniques
Mayo Clinic Children's Center uses specialized MRI protocols and a data-driven approach to evaluate children with epilepsy.
"A data-driven approach is essential for children with epilepsy," says Benjamin (Ben) H. Brinkmann, Ph.D., a biomedical engineer and clinical support scientist at Mayo Clinic's campus in Minnesota. "Many seizure types can be difficult for parents to recognize reliably. Seizures happening overnight are especially difficult to count reliably."
Several promising new devices, both wearable and minimally invasive, can help accurately identify and count seizures, to guide decisions about treatment.
Mayo Clinic also uses noninvasive electroencephalography (EEG) source imaging for pre-surgical evaluation. That technique identifies the source of abnormal EEG activity by calculating an inverse solution, using the individual's MRI scans to map the brain.
As described in the November 2021 issue of Brain Communications, Mayo Clinic researchers have demonstrated that ictal and interictal EEG source imaging has a high rate of agreement with intracranial EEG — and greater agreement than visual review alone.
When surgery is indicated, Mayo Clinic uses advanced technology such as intraoperative neuronavigation. Mayo Clinic's pediatric neurosurgeons have experience with a range of surgeries for epilepsy, including corpus callosotomy and hemispherectomy.
Ablación con láser de un tumor epileptógeno
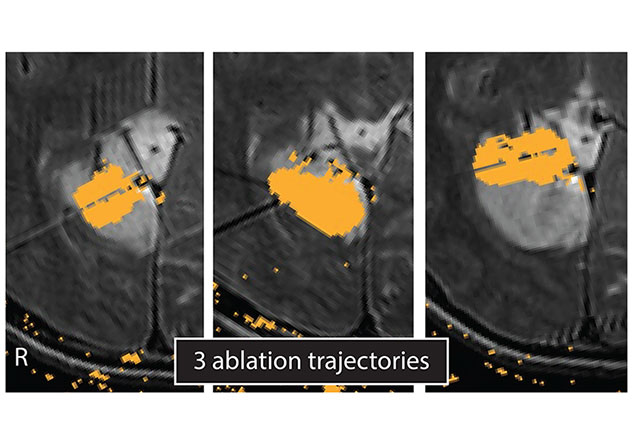
Ablación con láser de un tumor epileptógeno
Los mapas de daños muestran las tres trayectorias de ablación que se utilizaron en la terapia térmica intersticial inducida por láser de un tumor neuroepitelial disembrioplásico en un niño. El tumor ocasionaba convulsiones intratables.
"Less invasive options include laser interstitial therapy, which pinpoints and destroys a small portion of brain tissue without a large surgery or the need to damage otherwise healthy brain between the diseased area and the surface," says Kai J. Miller, M.D., Ph.D., a neurosurgeon at Mayo Clinic's campus in Minnesota.
Neurostimulation for children
Mayo Clinic specialists have experience with neurostimulation therapies that aren't commonly used to treat pediatric epilepsy. The options include responsive neurostimulation, deep brain stimulation and vagus nerve stimulation.
Children might also be candidates for Mayo Clinic's novel approach that aims to stop seizures before they start. Subthreshold cortical stimulation provides continuous electrical impulses to an area of seizure onset to suppress the generation of the abnormal seizure discharge. "This therapy has been safe and generally effective in children," Dr. Starnes says.
Mayo Clinic also uses two types of noninvasive neurostimulation:
- Transcranial magnetic stimulation for children with highly focal seizure origin sites
- Transcranial direct current stimulation for children with multiple seizure origin sites or a single, broad seizure origin site
"Noninvasive stimulation is potentially a very appealing option for children with drug-resistant epilepsy whose families are hesitant regarding a more invasive and permanent device implant," Dr. Starnes says.
Ketogenic diet
Mayo Clinic has pioneered the use of the ketogenic diet for children with medication refractory epilepsy. "Approximately 50% of children with medication refractory epilepsy respond to the ketogenic diet," says Katherine C. Nickels, M.D., a pediatric epileptologist at Mayo Clinic Children's Center in Minnesota. "But some syndromes and epilepsy causes have a greater response — for example, in reports of patients with intractable epilepsy due to tuberous sclerosis complex, approximately two-thirds responded."
A Mayo Clinic study published in the January 2021 issue of Epilepsia found that the ketogenic diet was the most effective treatment studied for children with myoclonic atonic epilepsy. The study, which included the largest reported retrospective cohort of children with that condition, found that overall response to the ketogenic diet was associated with a greater than 50% reduction in seizures in 79% of the individuals studied. Mayo Clinic has also studied the ketogenic diet's effectiveness for treating children with refractory epilepsy of genetic etiology, as well as for infants under the age of 12 months.
Mayo Clinic's care extends beyond seizure-reduction therapies. "We also look at comorbidities that often occur with epilepsy, including developmental problems, autism and other behavioral problems, sleep and movement disorders, and feeding difficulty," Dr. Wirrell says. "Our multidisciplinary team works to maximize quality of life both for children and their families."
For more information
Proposed classification and definition of epilepsy syndromes. International League Against Epilepsy.
Cox BC, et al. EEG source imaging concordance with intracranial EEG and epileptologist review in focal epilepsy. Brain Communications. 2021;3:fcab278.
Nickels K, et al. Epilepsy with myoclonic-atonic seizures (Doose syndrome): Clarification of diagnosis and treatment options through a large retrospective multicenter cohort. Epilepsia. 2021;62:120.
Refer a patient to Mayo Clinic.