Dec. 22, 2018
Mayo Clinic uses advanced intraoperative monitoring to prevent neurological complications during complex cervical spinal surgery. As a multidisciplinary center, Mayo Clinic can provide the team approach required for successful intraoperative monitoring.
"We work closely during these surgeries with a neurologist or physiatrist as well as an electrophysiology team. Our routine use of somatosensory- and motor-evoked potentials as well as electromyography allows us to monitor nerve pathways and alter our technique, to proactively prevent these patients from going on to develop neurological deficits," says Ahmad Nassr, M.D., an orthopedic surgeon at Mayo Clinic in Rochester, Minnesota.
Dr. Nassr estimates that intraoperative monitoring triggers an alert in about 25 percent of spinal surgeries. "The majority of these alerts may be subtle and related to limb positioning, not the surgery itself. However, failing to act on the alerts could result in significant harm to the patient," he says. "In more-complex surgeries, such as those for spinal cord compression, tumors and deformity surgery, the use of this monitoring can alert us to an impending problem and allow us to change our technique so as to avoid a neurological complication."
Proactive approach at all stages
Compresión de la columna vertebral

Compresión de la columna vertebral
La compresión espinal es evidente en la imagen preoperatoria.
The effort to prevent complications begins before surgery. Baseline neurological monitoring is performed to guide the positioning of the patient during the procedure. "We know that the position of the patient can impact his or her ability to undergo surgery safely," Dr. Nassr says. "Without that baseline monitoring and optimal positioning, there's a potential to injure the patient before we even start operating."
The intraoperative monitoring can identify even peripheral causes of nerve compression that will impact patients. "For example, if we have the arm tucked too hard at the patient's side, the monitoring can indicate that we're irritating the ulnar nerve at the elbow," Dr. Nassr says. "Although that sounds fairly minuscule, if patients are in that position for three or four hours, they can wake up with a fairly bad neurological deficit that has nothing to do with the cervical spine but with how the arm was positioned during surgery."
Cervical 5 (C5) palsy is less common, occurring in less than 10 percent of cervical spinal surgeries. But C5 palsy is usually detected only after surgery, as weakness in the deltoid and bicep become apparent.
Mayo Clinic routinely performs intraoperative C5 monitoring. "When we get an alert, we can do additional decompression around the C5 nerve root," Dr. Nassr says. "If C5 palsy does develop after surgery, we identify it early. We're recognizing its multiple causes and treating them aggressively to have more-favorable outcomes."
Treatment protocols developed at Mayo Clinic include physical therapy, electrical stimulation of the shoulder muscles and elevation of the shoulder to ease pressure on the brachial plexus. "Those efforts generally result in faster recovery for patients who develop C5 palsy, which can be an inevitable complication of some cervical spinal surgeries," Dr. Nassr says.
To further limit the risk of C5 palsy, Mayo Clinic resects the posterior longitudinal ligament (PLL) selectively. In a review published in the April 1, 2017, issue of Spine, Dr. Nassr and colleagues found that PLL resection is associated with a higher incidence of C5 palsy. "At Mayo, we try to resect the PLL only if it's necessary as part of the decompression," Dr. Nassr says.
Realineación de la columna vertebral
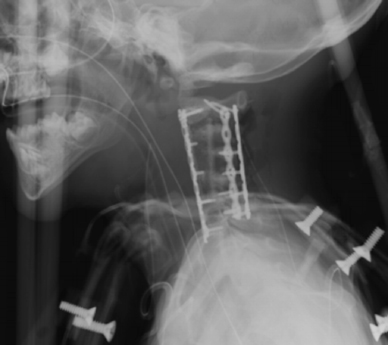
Realineación de la columna vertebral
La imagen postoperatoria inmediata muestra realineación de la columna vertebral.
Intraoperative monitoring is particularly important when patients aren't able to communicate with surgeons. Dr. Nassr cites a recent patient whose care he managed with A. Noelle Larson, M.D., a pediatric orthopedic surgeon at Mayo Clinic's campus in Minnesota. The 2-year-old patient had spinal cord compression — an unusual condition at that age — and was too young to cooperate with an intraoperative wake-up test. During the surgery, intraoperative monitoring triggered a C5 nerve alert. Drs. Nassr and Larson were able to alter their approach and avoid complications.
"The risks for patients are high in this type of case," Dr. Nassr says. "Outcomes like this aren't possible without intraoperative monitoring."
For more information
Nassr A, et al. Does resection of the posterior longitudinal ligament impact the incidence of C5 palsy after cervical corpectomy procedures?: A review of 459 consecutive cases. Spine. 2017;42:E392.