Jan. 07, 2021
As many as 50% of people with chronic constipation have functional defecation disorders and experience a condition called pelvic floor dysfunction. This condition affects people of all ages and typically involves impaired relaxation and coordination of pelvic floor and abdominal muscles that control the outlets of the bowel and bladder. Patients with pelvic floor dysfunction can experience abdominal pain, fecal incontinence as a result of laxative use, missed time at work and social isolation. Beyond these signs and symptoms, the condition is often accompanied by psychiatric issues, including anxiety and depression.
Based at Mayo Clinic's campus in Rochester, Minnesota, the Bowel Evacuation Disorders Program has a long, successful history of helping patients with pelvic floor dysfunction. The program's intensive curriculum involves retraining the pelvic floor muscles using biofeedback training and behavior modification. The program is coordinated by staff from Mayo Clinic's Physical Medicine and Rehabilitation who work closely with other professionals in Gastroenterology and Hepatology, Colon and Rectal Surgery, Urogynecology and Gynecology.
Functional defecation disorders
Although patients with functional defecation disorders don't always report being constipated, this diagnosis should be considered for anyone experiencing two or more symptoms from the Rome III criteria for constipation within a three-month period:
- Fewer than three bowel movements per week
- Straining during defecation
- Lumpy or hard stools
- Sensation of anorectal obstruction
- Sensation of incomplete defecation
- Manual digitation required to defecate
Some patients may require additional tests to confirm the diagnosis of pelvic floor dysfunction. Additional steps and tests that are helpful in making this diagnosis include physical examination, anorectal manometries and magnetic resonance (MR) proctogram.
"The physical examination can help assess baseline pelvic floor muscle tension as well as circumferential sphincter relaxation, posterior puborectalis release and expected perineal descent when bearing down," explains Karen L. Nehring, R.N., a physical medicine and rehabilitation nurse who works with these patients at Mayo Clinic's campus in Rochester, Minnesota. "Dyssynergia may manifest as nonrelaxation or paradoxical tightening."
According to Nehring, anorectal manometry with a balloon expulsion test is the diagnostic gold standard to identify pelvic floor dysfunction. A proctogram can assist in identifying structural abnormalities that may mimic or complicate pelvic floor issues. These might include pelvic organ prolapse, rectocele, enterocele or sphincteric incompetence.
Possible contributors
Several factors can contribute to pelvic floor dysfunction, including:
- Chronic holding behaviors, including those that begin in childhood or relate to specific jobs or family responsibilities
- Habitual pushing to "hurry the process" of toileting
- Muscle "guarding" in efforts to minimize incontinence or prolapse symptoms
- Pain-provoking events such as trauma, injury, disease or surgery affecting the abdominal or pelvic regions
- Childbirth with or without injury to the pelvic floor
- History of abuse
Pelvic floor muscle rehabilitation — The process
To participate in the Bowel Evacuation Disorders Program, patients must have sufficiently spared sensorimotor control through the pelvic floor muscles and obtain a referral from a physician at Mayo Clinic's campus in Minnesota.
Patients referred to the program are assessed by a nurse and triaged into one of the three available program formats that best meets their needs: once-weekly visits, a one-week program or a two-week program.
"Our nurses help determine the best interventions to use for each patient, addressing physical and psychological needs," says Heather L. Twing, R.N., ambulatory nurse manager in Physical Medicine and Rehabilitation at Mayo Clinic's campus in Rochester, Minnesota. "We strive to individualize the program to the specific needs of each patient."
For most patients, the process begins with neuromuscular rehabilitation, which teaches discrete control of the pelvic floor to produce a specific motion under direct consciousness of the patient. During these exercises, a nurse guides each patient to identify possible sensations associated with relaxation and tension, to isolate the pelvic floor from other muscle groups, and to identify strategies to sustain relaxation. Patients learn to develop new muscle memory through repetition of desired patterns and elimination of maladaptive patterns.
Sensor rectal
Sensor rectal
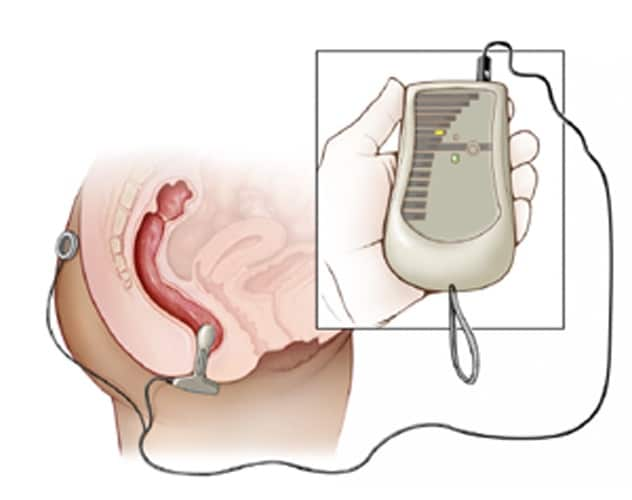
Un sensor de biorretroalimentación suave que se inserta en el conducto anal controla la tensión y relajación muscular mediante electromiografía y muestra información que los pacientes pueden ver en una pantalla.
Biofeedback-assisted muscle relaxation. A smooth biofeedback sensor inserted in the anal canal monitors muscle tension and relaxation through electromyography and displays feedback that patients can see on a screen. These exercises and the results provided by biofeedback can assist patients with baseline (day-to-day) relaxation, isolated muscle activation and pelvic floor strengthening exercises if indicated.
Practice with a rectal balloon. During this phase of the program, patients use a water-filled rectal balloon to simulate stool as it settles in the rectum and passes through the anal canal for evacuation. This activity provides sensory input to reinforce the correct sensations of rectal urge that should precede a bowel movement. Instruction in dynamic release focuses on the stages of pelvic floor descent, posterior puborectalis release and circumferential sphincter release. By learning to relax muscles to let go of the balloon without pushing, patients learn to correct maladaptive muscle patterns and reinforce desired patterns of release. These release patterns then reinforce the defecation reflex during actual bowel movements.
"These exercises help patients identify behaviors that may be contributing to symptoms while learning strategies for changing them," explains Nehring.
Additional skills and resources
Depending on the patient's needs, program staff can also arrange for patients to attend small group classes on stress management and general relaxation, normal bowel function, and wellness. The classes are offered in collaboration with Mayo Clinic's Barbara Woodward Lips Patient Education Center, Mayo Clinic Cancer Center and the Dan Abraham Healthy Living Center. Consults with dietitians and staff in Mayo Clinic's Pelvic Health Physical Therapy Program also are available to address diet, pain, sexual dysfunction, orthopedic contributors and other related issues.
Home program
After completing the initial program, the patient should plan to spend six to 12 weeks practicing with the exercises and equipment at home. This at-home practice helps patients incorporate relaxation skills into daily routines, reinforce behavioral changes, and use home biofeedback equipment to optimize and reinforce new muscle memory. During this phase, patients can contact a Mayo Clinic nurse for troubleshooting and questions.
Patient outcomes
Data obtained from 282 patients (27% male, 73% female, average age 43 years, range 15 to 79 years) after completion of the two-week program in 2019 indicate that the program helped many patients achieve positive outcomes. Immediately upon completion, participants reported improvement in their colorectal symptoms (94%) or urinary symptoms (90%). Additionally, 93% reported significant improvements in the impact of symptoms on their activities and relationships. Using the Global Rating of Change (GROC) scale:
- 60% of participants rated their change in knowledge as +7 (large change)
- 25% of participants rated their change in muscle control as +7
- 16% of participants rated their change in symptoms as +7
- 9% of participants reported no change in symptoms (0)
- 0.3% of participants reported being slightly worse (-3)
Nehring and Twing note that these data are encouraging and suggest that this program is assisting patients in developing knowledge and skills to address their symptoms and improve their quality of life.