Feb. 16, 2021
Approximately 200,000 anterior cruciate ligament (ACL) ruptures occur in the United States annually. Primary ACL reconstruction is recognized as a successful procedure, but failure has been shown to occur in approximately 10% of patients.
Mayo Clinic sports medicine surgeons routinely perform revision surgery for patients who have undergone one or more ACL reconstructions elsewhere, and have published extensively on this topic. Bruce A. Levy, M.D., an orthopedic surgeon specializing in sports medicine at Mayo Clinic in Rochester, Minnesota, discusses Mayo's approach to revision ACL surgery.
What factors does Mayo Clinic consider when evaluating a patient with a failed ACL reconstruction?
Imágenes previas a la operación
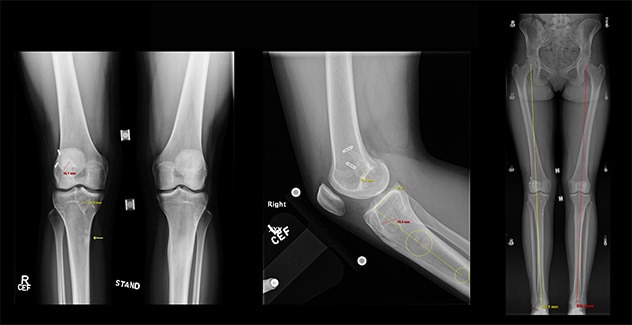
Imágenes previas a la operación
Las imágenes previas a la operación muestran un ensanchamiento excesivo de túneles y órbitas y no hay mala alineación con la pendiente normal.
Injerto óseo en fase I
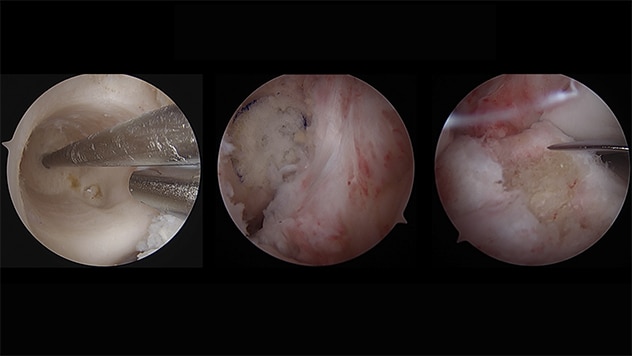
Injerto óseo en fase I
Injerto óseo femoral y tibial en fase I.
Reparación en etapa II
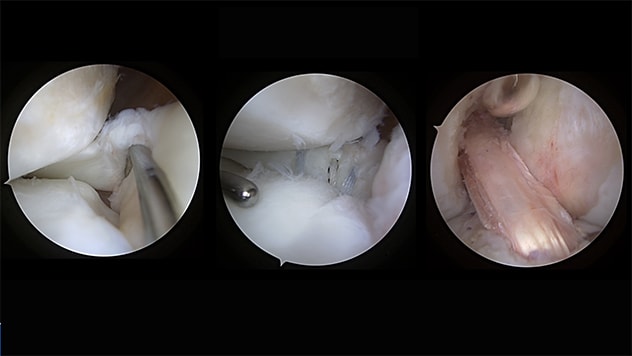
Reparación en etapa II
Desgarro de la raíz lateral en etapa II, reparación de la raíz lateral y repetición de la revisión del ligamento cruzado anterior espalda con espalda.
We focus on many factors including the status of the menisci, cartilage, alignment, tibial slope and other knee ligaments, as well as technical issues from the index surgery, such as the positioning of ACL sockets and tunnels. As our group described in 2013 in American Journal of Sports Medicine, all of these factors contribute to ACL failure and to the success of revision ACL surgery.
We routinely obtain hip-to-ankle AP X-rays to assess for any coronal plane malalignment. In addition, we obtain single leg knee-to-ankle lateral X-rays to assess for any sagittal plane malalignment as well as to look for excessive tibial slope.
There are numerous challenges to revision ACL surgery with regard to graft selection, timing of surgery, and whether or not the surgery can be performed in a single operation or multiple-staged surgeries. Optimal outcomes require a precise picture of how the ACL reconstruction failed. At Mayo Clinic, we have the imaging, surgical and physical therapy teams to manage extremely complex knee issues.
What causes do you commonly see?
Unfortunately, the most common cause for failure is related to technical issues from the primary ACL surgery, with malposition of the sockets and tunnels, particularly on the femoral side. Achieving the correct position can be tricky.
Meniscal tears are another contributing cause. Often the meniscus hasn't healed after the initial surgery, or lesions might have been overlooked during surgery, in particular meniscal root tears or meniscal ramp lesions. These lesions are often difficult to see on MRI. Unless the surgeon looks specifically for a ramp lesion at the time of ACL surgery, the lesion can be missed. Ramp tears can lead to rotational instability and put excessive strain on the ACL graft, causing it to fail.
Similarly, root tears of the lateral meniscus are often missed as well. Unless you probe for a root tear during surgery, you may miss it. Root tears also put tremendous forces on the ACL graft and can lead to rotational instability and graft failure.
What issues do you see with alignment?
Varus or valgus malalignment can put strain on an ACL graft, whatever the malalignment's cause — the patient's physiology, failed meniscal surgery or cartilage problems. At Mayo Clinic, we sometimes correct the alignment before performing revision ACL surgery, to prevent graft failure.
Excessive tibial slope also puts patients at much higher risk of early ACL reconstruction failure. The slope causes the tibia to move forward and the femur to fall backward, putting tremendous strain on the ACL. The greater the tibial slope, the higher the risk of graft failure — as our group found in a 2015 study in American Journal of Sports Medicine. At Mayo Clinic, we frequently perform osteotomies to correct both sagittal plane and coronal plane deformity.
Are these procedures performed in a single surgery, or staged?
A lot of factors help us to determine whether a single revision or a two- or multiple-stage revision would be best for a particular patient. For example, patients may require bone grafting of prior graft tunnels, and then have the ACL revision in a second stage. The bone grafting is an opportune time to do an osteotomy to correct the malalignment. Sometimes we can perform a biplanar osteotomy to correct both planes of deformity at once. This adds a fair amount of complexity to the procedure.
What other specialized procedures might be performed in conjunction with ACL revision surgery?
Patients who have lost a meniscus or have a significant cartilage defect and have a failed ACL can, in some circumstances, require a meniscus transplant or cartilage replacement surgery. Mayo Clinic has substantial experience with all of these procedures.
In addition, patients who receive revision ACL surgery might have other damaged ligaments. Mayo Clinic has vast experience treating posterior cruciate ligament, lateral collateral ligament, posterolateral and posteromedial corner injuries, as well as medial collateral ligament injuries. If any of those ligaments were missed in the initial knee surgery, they can be treated in the revision setting.
Recently, we recognized that patients needing ACL reconstruction who also have significant rotatory instability of the knee may have injuries in the anterolateral complex. There are several procedures that can be performed in the ACL revision setting, such as anterolateral ligament reconstruction and iliotibial band tenodesis, to control that rotation.
What research is underway?
Several Mayo Clinic orthopedic surgeons are members of the Multicenter ACL Revision Study (MARS) Group, which has authored a series of reports on topics including predictors of clinical outcomes, published in Journal of Orthopaedic Research in 2020. At Mayo Clinic, we also are evaluating surgical techniques for ACL reconstruction, as well as optimal approaches to multiligament knee reconstruction. The goal is to ensure patients of all activity levels, from professional to recreational, have the surgeries that meet their individual needs. We want our patients to be able to return to the activities they enjoy.
Can you share a case with us?
A 17-year-old female came to see us after two failed ACL surgeries. Her alignment, tibial slope and cartilage were all normal. Unfortunately, both previous reconstructions were performed with allograft (cadaver) tissue, which has been shown to have significantly higher failure rates in young patients compared with autograft (the patient's own tissue). The patient also had an unrecognized complete disruption of her lateral meniscal root and excessively widened tunnels and sockets.
This case required a two-stage approach: Stage 1 consisted of bone grafting, followed by second-stage repeat revision ACL reconstruction with patellar tendon autograft, lateral meniscal root repair and iliotibial band tenodesis. Two years after the surgery, she resumed all activities and plays collegiate volleyball.
For more information
Griffith TB, et al. Outcomes of repeat revision anterior cruciate ligament reconstruction. American Journal of Sports Medicine. 2013;41:1296.
Christensen JJ, et al. Lateral tibial posterior slope is increased in patients with early graft failure after anterior cruciate ligament reconstruction. American Journal of Sports Medicine. 2015;43:2510.
MARS Group. Predictors of clinical outcome following revision anterior cruciate ligament reconstruction. Journal of Orthopaedic Research. 2020;38:1191.