May 22, 2021
The standard of care for patients with intermediate or high-risk nonmuscle invasive bladder cancer is intravesical, induction bacillus Calmette-Guerin (BCG) treatment. Unfortunately, more than half the patients will develop a recurrence within a year of treatment, and many will develop BCG-unresponsive disease.
Updated guidelines by the American Urological Association offer patients with BCG-unresponsive bladder cancer three main treatment options:
- Radical cystectomy in patients who are fit and willing to undergo radical surgery
- Salvage intravesical chemotherapy
- Pembrolizumab in patients with carcinoma in situ with or without papillary tumor
Pembrolizumab received U.S. Food and Drug Administration approval for treatment of patients with BCG-unresponsive carcinoma in situ in January 2020. Pembrolizumab may offer effective treatment to a subset of patients but is associated with high costs (more than $100,000 a year) and the potential for significant side effects.
Carcinoma de vejiga in situ
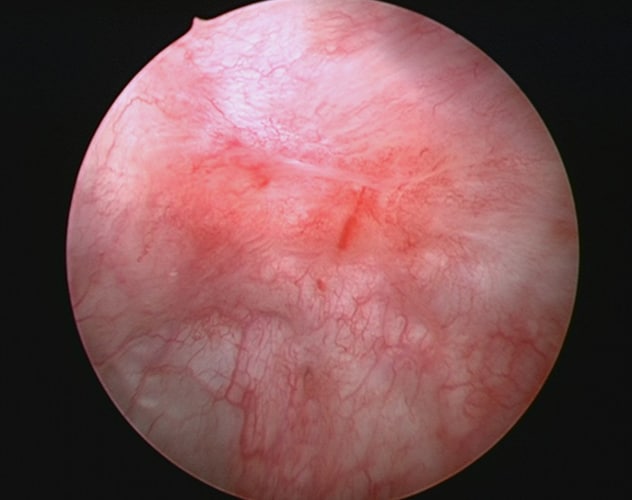
Carcinoma de vejiga in situ
La imagen cistoscópica muestra un carcinoma de vejiga in situ.
Given these treatment options with variable effectiveness and differing costs, a multi-institutional team, led by Stephen A. Boorjian, M.D., a urologic oncologist at Mayo Clinic in Rochester, Minnesota, conducted a study to compare the cost-effectiveness of pembrolizumab with radical cystectomy and salvage intravesical chemotherapy (in this case, gemcitabine and docetaxel). The authors evaluated patients who would be eligible for any of these treatments — patients with BCG-unresponsive carcinoma in situ with or without papillary tumor.
Kevin M. Wymer, M.D., chief resident and Mayo Clinic scholar in endourology at Mayo Clinic in Rochester, Minnesota, notes: "There is much enthusiasm regarding the use of immunotherapy or checkpoint inhibitors, such as pembrolizumab, in urologic cancers. As is often the case with new medications, however, their widespread use can be restrained by costs. Of course, if the benefits of a medication outweigh the risks and costs associated with the morbidities of other treatments, even an expensive medication can become cost-effective."
Methodology
A Markov model was used to evaluate the cost-effectiveness of pembrolizumab relative to cystectomy and salvage intravesical chemotherapy. Cost-effectiveness was assessed for two index patients who may consider pembrolizumab in a real-world setting:
- Index patient 1 is willing and fit to undergo radical cystectomy.
- Index patient 2 is unwilling or unfit to undergo radical cystectomy.
All costs were based on 2019 U.S. Medicare reimbursements and were discounted at a 3% annual rate. The study looked at five-year oncologic outcomes, toxicity rates and utility values from the literature. Univariable and multivariable sensitivity analyses were performed. A threshold of $100,000 per additional quality-adjusted life year (QALY) was used to define cost-effectiveness.
Results: Index patient 1
At five years, mean costs per patient were $39,367 for cystectomy, $43,488 for salvage intravesical chemotherapy and $191,297 for pembrolizumab. Five-year effectiveness was 4.29, 4.32 and 4.39 QALYs for cystectomy, salvage intravesical chemotherapy and pembrolizumab, respectively.
Pembrolizumab was not cost-effective when compared with cystectomy ($1,403,008 per QALY) and salvage intravesical chemotherapy ($2,011,923 per QALY). Salvage intravesical chemotherapy was likewise not cost-effective compared with cystectomy ($118,324 per QALY).
Pembrolizumab became cost-effective compared with cystectomy only in the setting in which the three-month price decreased from its actual price of $43,131 to $2,652 — which represents a 93% decline in the current price.
Salvage intravesical chemotherapy became the most cost-effective in several situations, including the following:
- Two-year probability of metastasis after treatment with salvage intravesical chemotherapy decreased from 6.1% (expected probability) to 5.9% or less.
- Two-year probability of intravesical recurrence decreased from 57.5% (expected probability) to 55% or less.
- Cost of cystectomy increased from $11,527 to $13,228 or more.
- Five-year intravesical recurrence after salvage intravesical chemotherapy decreased from 73.5% (expected rate) to 70% or less.
- Three-month cost of chemotherapy decreased from $1,038 to $760 or less.
In multivariable sensitivity analyses of 100,000 microsimulations, at a willingness-to-pay threshold of $100,000, cystectomy was cost-effective in 54% of simulations, chemotherapy in 46%, and pembrolizumab in 0%. Even when the willingness-to-pay threshold was increased to $500,000, pembrolizumab was still not cost-effective.
When the intervals of follow-up after treatment were adjusted, salvage intravesical chemotherapy was cost-effective at shorter intervals (less than five years), whereas cystectomy was more cost-effective after five years.
Results: Index patient 2
At five years, mean costs per patient were $38,192 for salvage intravesical chemotherapy and $189,902 for pembrolizumab. Five-year effectiveness was 4.21 and 4.35 QALYs for salvage intravesical chemotherapy and pembrolizumab, respectively.
Pembrolizumab was not cost-effective when compared with salvage intravesical chemotherapy ($1,073,240 per QALY).
Pembrolizumab became cost-effective only when the three-month cost was hypothetically decreased to less than $4,263.
The results of multivariable sensitivity analyses demonstrated that pembrolizumab was cost-effective in 0% of microsimulations.
Radical cystectomy remains the gold standard
Given the current relatively high cost of pembrolizumab, its use for patients with BCG-unresponsive carcinoma in situ is not cost-effective when compared with the gold standard of cystectomy or the alternative of salvage intravesical chemotherapy.
Dr. Boorjian notes: "This type of analysis may be utilized to evaluate novel therapies in this disease space. We need to continue to pursue therapies and combinations of therapy to maximize the quality and length of life for our patients with bladder cancer. This study provides an assessment of existing treatments for BCG-unresponsive bladder cancer. Presently, radical cystectomy remains the gold standard treatment here."
Study results were published in The Journal of Urology in 2021.
For more information
Wymer KM, et al. Cost-effectiveness analysis of pembrolizumab for bacillus Calmette-Guérin-unresponsive carcinoma in situ of the bladder. The Journal of Urology. 2021;205:1326.