Diagnosis
Lymphoma FAQs
Hematologist Stephen Ansell, M.D., answers the most frequently asked questions about lymphoma.
Well, many times we don't actually know. We do know what exactly happens in the cells. We can see that the cells undergo a genetic change. And as they do that, they may grow quicker than they should, and they may persist and not die off like they should. That causes them to slowly accumulate over time. But exactly what brought about that genetic change, we don't always know.
This is not a disease that's passed down in families, although families can be more susceptible. But we think there are some susceptibility genes that may put you at risk for being more likely to get lymphoma. That does, however, require something else to happen, often in the way of exposures to toxins or viruses or something else.
Well, I think it's important to recognize what the goals of treatment are. Low-grade lymphomas have an advantage in that they can take a very long time to cause any symptoms, and certainly a very long time to put the patient's health at risk. However, we do not have a curative treatment that will fix the cancer right away. So we want to weigh up the potential risks and side effects that come with treatment compared to, clearly, the risks and side effects that come from the cancer. So, if you have a cancer that is very low-grade, growing very slowly, giving you no symptoms, we would hold off on treatment and only initiate it when you truly need it.
Well, important to know that chemotherapy may have two components. Chemotherapy, or chemical drugs that are targeting the cancer, immunotherapy, or antibody treatments that are going after proteins that are on the outside of the cancer or lymphoma cells. The goal of chemotherapy is to kill quickly- growing cells, which is a good thing because lymphoma, many times, those cells are growing quickly. The challenge, however, is there are healthy cells that may also be growing quickly. Immunotherapy, as I mentioned, binds or attacks proteins on the outsides of cells. But some of the lymphoma cells and some of the normal cells have the same proteins. So those cells may be depleted, and your immune system may become a little bit more suppressed as one of the potential side effects of therapy.
Well, I really wish that was true. Unfortunately, that's not exactly correct. There isn't a treatment or exercise program that directly targets or goes after the lymphoma cells. Generally, however, what a healthy balanced diet and a good exercise program is doing is improving your general well-being, improving your immune system function, and allowing you to tolerate the chemotherapy and fight against the cancer to a greater degree. The good news is that many studies have shown that a healthy patient who's in good shape actually has a better outcome when receiving treatment for lymphoma. So that's a strong motivation for you to be healthy by eating well and exercising regularly.
Get as much information as you can. Partner with your physician, your nurse practitioner, your PA and other members of the team and ask questions. The goal moving forward is for you to have the best outcome possible. So that sharing of information between your team and you is critical to your outcome and the best results we could hope for.
Bone marrow exam
Bone marrow exam
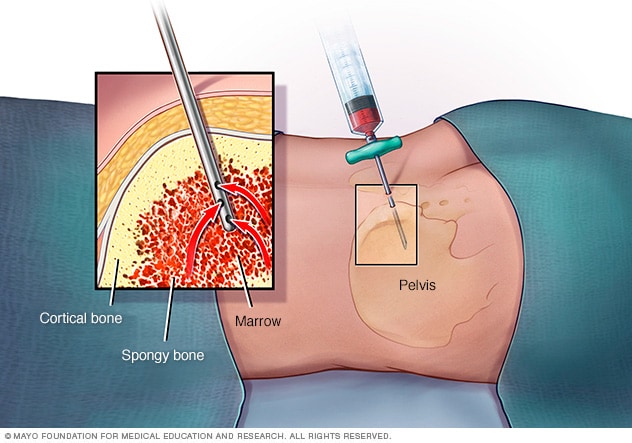
In a bone marrow aspiration, a healthcare professional uses a thin needle to remove a small amount of liquid bone marrow. It is usually taken from a spot in the back of the hip bone, also called the pelvis. A bone marrow biopsy is often done at the same time. This second procedure removes a small piece of bone tissue and the enclosed marrow.
Diagnosis of lymphoma often begins with a physical exam. This exam checks for swollen lymph nodes in the neck, underarms and groin and an enlarged spleen or liver. Other tests and procedures include blood tests, imaging tests and taking a sample of tissue for lab testing.
Blood tests
Blood tests can sometimes show whether lymphoma cells are present. Blood tests may be used to test for viruses, including HIV, hepatitis B virus and hepatitis C virus. Blood tests also measure levels of lactate dehydrogenase (LDH), which is often higher in people with lymphoma.
Imaging tests
Imaging tests make pictures of the body. They can show the location and extent of lymphoma. Tests might include MRI, CT and positron emission tomography (PET) scans.
Biopsy
Your healthcare professional may suggest a lymph node biopsy or a biopsy of other tissue to look for cancer cells. A biopsy is a procedure to remove a sample of tissue for testing in a lab. A lymph node biopsy involves removing all or part of a lymph node. A sample may be taken from other parts of the body depending on symptoms and imaging test results. In the lab, tests may show whether you have lymphoma.
Bone marrow aspiration and biopsy
Bone marrow aspiration and biopsy are procedures to collect cells from the bone marrow for testing. Bone marrow is the soft matter inside bones where blood cells are made. Bone marrow has a solid part and a liquid part.
In a bone marrow aspiration, a needle is used to collect a sample of the fluid. In a bone marrow biopsy, a needle is used to collect a small amount of the solid tissue. Most often, the samples are taken from the hip bone. The samples go to a lab for testing. In lymphoma, this procedure can show if the bone marrow is involved and help determine the cancer's extent.
Lumbar puncture
A lumbar puncture is a procedure to collect fluid from around the spinal cord. A lumbar puncture, also called a spinal tap, uses a needle. A healthcare professional inserts the needle between two bones in the lower back and draws out some of the fluid that surrounds the brain and spinal cord. This fluid is called cerebrospinal fluid. The fluid goes to a lab where it's tested for cancer cells.
For lymphoma, a lumbar puncture may be done if you have neurological symptoms. It also may be done if you are at higher risk of lymphoma of the central nervous system.
Upper endoscopy
An upper endoscopy is a procedure to look at the inside of the esophagus, stomach and first part of the small intestine. A thin, tubelike instrument with a light and a lens for viewing, called an endoscope, is inserted through the mouth and passed down the throat. Tools are passed through the tube to remove a sample of tissue for testing. It may be used if your healthcare professional thinks you have lymphoma in the stomach.
Testing lymphoma cells in the lab
Lymphoma cells collected from a biopsy or a bone marrow aspiration and biopsy go to a lab for testing. In the lab, specialized tests look for specific things about the cells. The healthcare team uses the results to find out the type of lymphoma that you have.
To learn whether the cells are Hodgkin lymphoma cells, the healthcare professionals in the lab look for:
- Proteins on the surface of the cancer cells. Lymphoma cells have certain proteins on their surfaces that help identify them. These proteins are known as markers. These markers can help identify the type of lymphoma.
- Changes in the cancer cell DNA. Cancer happens when cells get changes in their DNA. A cell's DNA holds the instructions that tell the cell what to do. Some lymphomas have a gene change that causes their DNA to rearrange. This is known as translocation. Some genes also may be missing parts of their DNA, called deletion. These gene changes cause the cells to multiply rapidly.
More Information
Treatment
Treatments for lymphomas may include a "watch and wait" approach, chemotherapy, immunotherapy, radiation therapy, targeted therapy, and clinical trials. Treatments also may include CAR-T cell therapy, bone marrow transplant, also called bone marrow stem cell transplant, and treatments for cutaneous lymphomas. Which treatment is best for you depends on the type of lymphoma you have and the extent of your cancer, called the stage. Your healthcare team also considers how quickly the cancer is growing, your overall health and what you prefer.
Watch and wait
If your lymphoma doesn't cause symptoms, you might not need treatment right away. Instead, you may have checkups every few months. The checkups help your healthcare team watch your condition to see if your cancer is growing.
Chemotherapy
Chemotherapy treats cancer with strong medicines. There are many chemotherapy medicines. Most chemotherapy medicines are given through a vein. Some come in pill form.
Chemotherapy may be a treatment for some types of lymphoma. You may take a combination of chemotherapy medicines. Chemotherapy also may be combined with immunotherapy or other medicines. Chemotherapy may be an option when other treatments haven't worked, known as refractory lymphoma, or for cancer that comes back after treatment, called relapsed lymphoma.
Immunotherapy
Immunotherapy for cancer is a treatment with medicine that helps the body's immune system kill cancer cells. The immune system fights off diseases by attacking germs and other cells that shouldn't be in the body. Cancer cells survive by hiding from the immune system. Immunotherapy helps the immune system cells find and kill the cancer cells.
Immunotherapy may be a treatment for some types of lymphoma. It may be combined with chemotherapy or other medicines. Immunotherapy also may be used for refractory or relapsed lymphoma.
Radiation therapy
Radiation therapy for cancer is a treatment that uses powerful energy beams to kill cancer cells. The energy can come from X-rays, protons or other sources. During radiation therapy, you lie on a table while a machine moves around you. The machine directs radiation to precise points in your body.
Radiation therapy may be a treatment for some types of lymphoma. It may be combined with chemotherapy or other medicines. Radiation therapy also may be used to ease symptoms and improve quality of life for people with some types of lymphoma.
Targeted therapy
Targeted therapy for cancer is a treatment that uses medicines that attack specific chemicals in cancer cells. By blocking these chemicals, targeted treatments can cause cancer cells to die.
Targeted therapy may be a treatment for some types of lymphoma. It also may be an option for some refractory or relapsed B-cell lymphomas.
Clinical trials
Clinical trials are studies of new treatments. These studies provide a chance to try the latest treatments. The risk of side effects might not be known. Talk with your healthcare team about the possibility of joining a clinical trial.
CAR-T cell therapy
Chimeric antigen receptor (CAR)-T cell therapy trains the immune system cells to fight lymphoma. This treatment begins with removing some white blood cells, including T cells, from the blood.
The cells are sent to a lab. In the lab, the cells are treated so that they make special receptors. The receptors help the cells recognize a marker on the surface of the lymphoma cells. Then the cells go back into the body. They find and destroy lymphoma cells.
CAR-T cell therapy may be an option for some refractory or relapsed lymphomas.
Bone marrow transplant
A bone marrow transplant, also called a bone marrow stem cell transplant, involves putting healthy bone marrow stem cells into the body. These cells replace cells hurt by chemotherapy and other treatments. Stem cells can come from your own body, called an autologous transplant. Stem cells also can come from a donor, called an allogeneic transplant.
A bone marrow transplant may only be an option for some types of lymphoma and for people who are younger and in good health. Chemotherapy is typically done before the transplant to suppress the immune system and bone marrow.
Treatments for cutaneous lymphomas
Treatments for cutaneous lymphomas may include topical medicines and phototherapy. Topical medicines are placed directly on the patches or plaques on the skin. They may include corticosteroids, retinoids and topical chemotherapy. Phototherapy uses lights combined with medicines to treat some cancers of the skin.
Monitoring after treatment
After treatment is complete, you may have frequent follow-up appointments to see if the cancer has come back, known as a relapse. You may have repeat blood and imaging tests and, if needed, biopsies, to check for relapse.
Side effects of treatment
Treatments for lymphoma may have side effects. These may include nausea, vomiting, fatigue, fever, rash, diarrhea, infection and more.
Harmful side effects from treatments may include:
- Bone marrow suppression. When the bone marrow is suppressed, it can't produce enough blood cells, including white blood cells. White blood cells help fight infections, so with a lower amount, you are at a higher risk of infections.
- Febrile neutropenia. Febrile neutropenia is a serious condition that can happen in people being treated for cancer. Febrile means having a fever. Neutropenia means having a low number of neutrophils, which are a type of white blood cell that helps fight infections. In febrile neutropenia, the body is trying to fight an infection but doesn't have enough neutrophils.
- Medicine toxicity. Some medicines used to treat cancer can be harmful to the body. They can cause organ damage and other issues. Whether a medicine is toxic depends on the type and how much you take. There are many different medicine options. Your healthcare team can work with you to find the best medicines for you.
- Reactivating viruses. If you have had a viral infection in the past such as hepatitis B or hepatitis C, some treatments can cause the virus to become active again. This can lead to liver inflammation, liver damage and other complications.
- Tumor lysis syndrome. Tumor lysis syndrome is a serious condition that can happen when cancer cells break down quickly after treatment. When these cells die, they release substances into the bloodstream that can overwhelm the body. This can lead to issues with the kidneys and other organs. You may take medicines to treat or prevent harmful side effects.
- Infertility. Some lymphoma medicines can cause issues with fertility. If you are concerned about fertility, talk about your options with your healthcare professional before beginning treatment.
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Coping and support
With time, you'll likely find what helps you cope with the uncertainty and worry of a cancer diagnosis. Until then, you may find that it helps to:
Learn enough about lymphoma to make decisions about your care
Ask your healthcare team about your cancer, including your test results, treatment options and, if you want, your prognosis. As you learn more about lymphoma, you may become more confident in making treatment decisions.
Keep friends and family close
Keeping your close relationships strong can help you deal with your lymphoma. Friends and family can provide the practical support you may need, such as helping take care of your home if you're in the hospital. And they can serve as emotional support when you feel overwhelmed by having cancer.
Find someone to talk with
Find someone who is willing to listen to you talk about your hopes and worries. This person may be a friend or family member. The concern and understanding of a counselor, medical social worker, clergy member or cancer support group also may be helpful.
Ask your healthcare team about support groups in your area or contact organizations such as the American Cancer Society, Blood Cancer United and the Lymphoma Research Foundation. Find support online through Mayo Clinic Connect, which is a community where you can connect with others for support, practical information and answers to everyday questions.
Follow us on Twitter
@MayoCancerCare
Preparing for your appointment
Make an appointment with a healthcare professional if you have any symptoms that worry you.
If your healthcare professional thinks you might have lymphoma, you may be referred to a doctor who specializes in diseases that affect blood cells, called a hematologist. If a cancer diagnosis is made, you also may be referred to a doctor who specializes in treating cancer, called an oncologist.
Because appointments can be brief, it's a good idea to be prepared. Here's some information to help you get ready.
What you can do
- Be aware of anything you need to do ahead of time. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet.
- Write down symptoms you have, including any that may not seem related to the reason for which you scheduled the appointment.
- Write down important personal information, including major stresses or recent life changes.
- Make a list of all medicines, vitamins and supplements you're taking and the doses.
- Take a family member or friend along. It can be hard to remember all the information you get during an appointment. Someone who goes with you may remember something that you missed or forgot.
- Write down questions to ask your healthcare team.
For lymphoma, some basic questions to ask include:
- Do I have lymphoma?
- What type of lymphoma do I have?
- What is the stage of my lymphoma?
- Has my lymphoma spread to other parts of my body?
- Will I need more tests?
- What are the treatment options?
- How much does each treatment prolong my life or increase my chances of a cure?
- What are the potential side effects of each treatment?
- How will each treatment affect my daily life?
- Is there one treatment option you believe is the best?
- What would you recommend to a friend or family member in my situation?
- Should I see a specialist?
- Are there any brochures or other printed material that I can take with me? What websites do you recommend?
- What will determine whether I should plan for a follow-up visit?
Don't hesitate to ask other questions.
What to expect from your doctor
Be prepared to answer questions, such as:
- When did your symptoms begin?
- Do your symptoms happen all the time or do you have them now and then?
- How bad are your symptoms?
- What, if anything, seems to make symptoms better?
- What, if anything, seems to worsen your symptoms?
- Have you had any fevers, night sweats or weight loss?
- Have you noticed any lumps, swelling or pain anywhere in your body?
- Have you had any chest pain, coughing or trouble breathing?
- Have you had any recent infections?
- Do you have any other health conditions, such as diabetes, heart disease or kidney disease?
- What are your biggest worries about your diagnosis or treatment?
Sept. 16, 2025