Overview
Chambers and valves of the heart
Chambers and valves of the heart
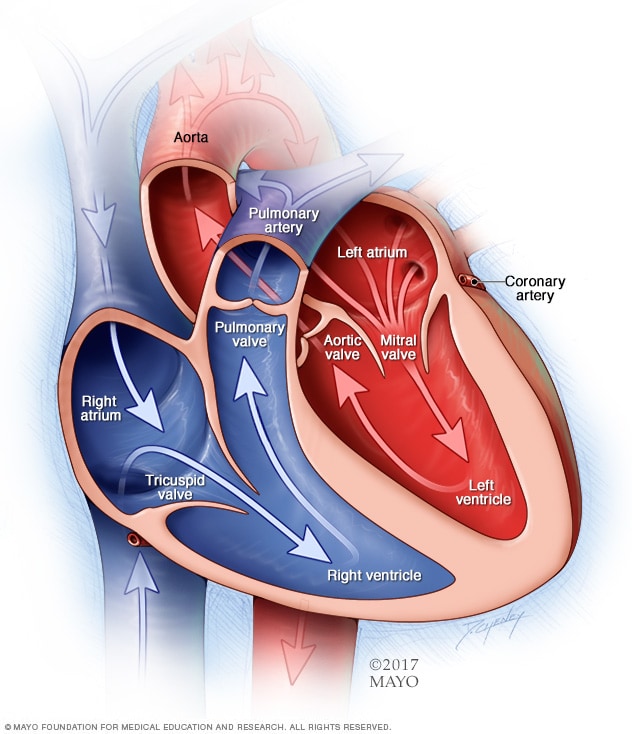
A typical heart has two upper and two lower chambers. The upper chambers, the right and left atria, receive incoming blood. The lower chambers, the more muscular right and left ventricles, pump blood out of the heart. The heart valves help keep blood flowing in the right direction.
Pulmonary valve repair and pulmonary valve replacement are surgeries to treat a diseased or damaged pulmonary valve.
The pulmonary valve is one of four valves that control blood flow in the heart. The valve is between the lower right heart chamber and the artery that brings blood to the lungs, called the pulmonary artery. The pulmonary valve has flaps, called cusps, that should open and close once during each heartbeat.
A diseased or damaged pulmonary valve can block blood flow from the heart to the lungs. Pulmonary valve repair and pulmonary valve replacement can help improve blood flow and reduce symptoms of heart valve disease.
Products & Services
Types
Why it's done
Pulmonary valve regurgitation

Pulmonary valve regurgitation
In pulmonary valve regurgitation, the pulmonary valve fails to close. As a result, blood can flow backward.
Pulmonary valve repair and pulmonary valve replacement are done to treat a damaged or diseased pulmonary valve.
Types of pulmonary valve disease that may need treatment with pulmonary valve repair or pulmonary valve replacement include:
- Pulmonary valve regurgitation. The valve cusps may not close tightly, causing blood to leak backward. Blood goes backward into the heart instead of to the lungs.
- Pulmonary valve stenosis. The valve cusps become thick or stiff. Sometimes they join together. The valve opening becomes narrowed. The heart must work harder to pump blood to the lungs.
- Pulmonary atresia. The pulmonary valve isn't formed. A solid sheet of tissue blocks the blood flow between the heart chambers.
The decision to repair or replace a damaged pulmonary valve depends on many things, including:
- The severity, also called stage, of pulmonary valve disease.
- Symptoms.
- Age and overall health.
- Whether the condition is getting worse.
- Whether surgery is needed to correct another valve or heart condition.
Surgeons usually suggest pulmonary valve repair when possible. Repair saves the heart valve and helps the heart work better. If you need surgery for another heart condition, a surgeon might do valve repair or replacement at the same time.
To get the best results, pulmonary valve repair or replacement should be done at medical centers with medical teams experienced in heart valve surgery.
Risks
All surgeries have risks. Risks of pulmonary valve repair and replacement depend on:
- Your health.
- The type of surgery.
- The expertise of the surgeons and healthcare team.
Possible risks of pulmonary valve repair and pulmonary valve replacement are:
- Bleeding.
- Blood clots.
- Failure of a replacement valve.
- Heart attack.
- Irregular heart rhythms, called arrhythmias.
- Infection.
- Stroke.
- Possible need for a pacemaker.
How you prepare
 Pulmonary valve disease consultation at Mayo Clinic
Pulmonary valve disease consultation at Mayo Clinic
Your Mayo Clinic treatment team discusses any questions you might have about your pulmonary valve repair or pulmonary valve replacement procedure at Mayo Clinic.
Before pulmonary valve repair or replacement, your surgeon and treatment team discuss your surgery with you and answer any questions. Before you go to the hospital, talk with your family or loved ones about your hospital stay. Discuss any help you may need when you return home.
Food and medications
Before you have pulmonary valve surgery, talk with your care team about:
- All medicines you take and whether you can take them before your surgery.
- Allergies or reactions you've had to medicines.
- When you should stop eating or drinking before your surgery.
Clothing and personal items
Your healthcare team may suggest that you bring several items to the hospital, including:
- A list of the medicines you take. Include the dosages.
- Eyeglasses, hearing aids or dentures.
- Personal care items such as a brush, a comb, a shaving kit and a toothbrush.
- Loose, comfortable clothing.
- A copy of your advance directive. This is a legal document. It includes instructions about the kinds of treatments you want or don't want in case you can't tell someone.
- Items that help you relax, such as portable music players or books.
Do not wear:
- Contact lenses.
- Dentures.
- Eyeglasses.
- Jewelry.
- Nail polish.
What you can expect
Before the procedure
Before pulmonary valve repair or replacement, a member of your care team places an IV into your forearm or hand. Fluids and medicines go through the IV.
A member of your care team may shave hair from the area of the body where the surgical cuts, called incisions, are made. A special soap might be used to wash your skin to help prevent infection.
During the procedure
You get a combination of medicines to put you in a sleep-like state during the surgery, so you won't feel pain. This is called general anesthesia.
You are connected to a heart-lung bypass machine, which keeps blood moving through the body during the surgery.
Pulmonary valve repair
Pulmonary valve repair is usually done as open-heart surgery. This involves opening the chest bone, called a sternotomy. Surgeons wire the bone back together after the surgery.
During pulmonary valve repair, a surgeon might:
- Separate valve flaps that have fused.
- Make one or more new valve flaps from your own heart tissues.
- Remove any patches that may have been placed during earlier heart surgeries and bring the valve flaps together to create a working valve.
- Reshape or remove tissue to let the valve close tighter.
- Tighten or strengthen the ring around the valve, called the annulus.
Minimally invasive pulmonary valve repair
If the pulmonary valve has a narrowed opening, a type of heart valve repair called balloon valvuloplasty may be done. It's a minimally invasive surgery. It most often involves smaller cuts and a shorter hospital stay than traditional open-heart surgery does.
During balloon valvuloplasty, a catheter with a balloon on the tip is placed into an artery in the arm or groin. Then it is guided to the pulmonary valve. The balloon is inflated, which widens the valve opening. Then the balloon is deflated. The catheter and balloon are removed.
Balloon valvuloplasty is often used to treat infants and children with pulmonary valve stenosis. But the valve tends to narrow again in adults who have had the treatment. More procedures may be needed to treat the narrowed pulmonary valve over time.
Pulmonary valve replacement
Pulmonary valve replacement: Biological valve

Pulmonary valve replacement: Biological valve
In a biological pulmonary valve replacement, a valve made from cow, pig or human heart tissue replaces the damaged valve.
If the pulmonary valve can't be repaired and other treatments aren't an option, the valve might need to be replaced. To replace a heart valve, a surgeon removes the heart valve and replaces it with a mechanical valve or a valve made from cow, pig or human heart tissue. Valves made from tissue are called biological valves.
If you have a mechanical valve, you need to take blood-thinning medicines for life to prevent blood clots. Biological valves break down over time and may need to be replaced again. You and your healthcare team discuss the risks and benefits of each type of valve to choose the one that's best for you.
Pulmonary valve replacement may be done using open-heart surgery or minimally invasive methods, which involve smaller surgical cuts than those used in open-heart surgery. Talk with your surgeon and treatment team about the best option for you.
Minimally invasive pulmonary valve replacement
Pulmonary valve-in-valve replacement

Pulmonary valve-in-valve replacement
In a transcatheter valve-in-valve procedure, a heart surgeon inserts a thin, hollow tube called a catheter into a blood vessel, usually in the groin. The catheter is then guided to the heart. A replacement valve goes through the catheter. A balloon on the tip of the catheter expands to press the new valve into the existing pulmonary valve.
Minimally invasive pulmonary valve replacement helps lower the number of open-heart surgeries that a person needs. The most common type of minimally invasive pulmonary valve replacement is transcatheter pulmonary valve replacement. It also is called percutaneous pulmonary valve replacement.
In this type of pulmonary valve replacement, the surgeon places a thin, flexible tube called a catheter into a large blood vessel in the groin or chest. The surgeon guides the catheter to the heart. A replacement pulmonary valve goes through the catheter. A balloon on the tip of the catheter expands to press the new pulmonary valve into place.
A transcatheter procedure also may be used to place a new pulmonary valve into a previously replaced valve that no longer works. This is called a valve-in-valve procedure.
After the procedure
After pulmonary valve repair or replacement, you usually spend a day or more in the hospital's intensive care unit (ICU). You get fluids and medicines through an IV. Other tubes drain urine from the bladder and fluid and blood from the chest. You might get oxygen through a mask or a small plastic tube next to your nose.
After staying in the ICU, you go to a regular hospital room for a few days. The time you spend in the hospital can vary depending on your health and type of heart valve surgery.
During your hospital stay, your healthcare team:
- Checks your blood pressure, breathing and heart rate.
- Watches for signs of infection.
- Works with you to manage any pain you have.
You may be asked to walk regularly. This helps you slowly become more active. You are usually asked to cough and to do breathing exercises as you recover too.
You get instructions to follow as you recover from pulmonary valve surgery, such as how to:
- Manage pain and other side effects after your surgery.
- Properly care for your incisions.
- Take your medicines.
- Watch for symptoms of infection in your incisions.
Results
The results of pulmonary valve repair and replacement can depend on the skill and experience of the surgeons and medical center.
After pulmonary valve repair or replacement, you need regular health checkups to make sure the new or repaired valve is working properly. Your care team tells you when you can return to daily activities, such as working, driving and exercising.
After heart valve surgery, it's important to keep the heart healthy. Try these tips:
- Get regular exercise.
- Control your weight.
- Eat a healthy diet.
- Manage stress.
- Do not smoke or use tobacco
- Get 7 to 8 hours of sleep daily.
Your care team also may suggest a personalized learning and education program called cardiac rehabilitation. Cardiac rehab focuses on exercise, a heart-healthy diet, stress management and a gradual return to usual activities. Cardiac rehabilitation usually starts in the hospital. The program typically continues for a few weeks or months after you return home.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.