Mayo Clinic's approach
Teamwork
 Pancreas transplant consultation
Pancreas transplant consultation
Pancreas transplant consultation at Mayo Clinic
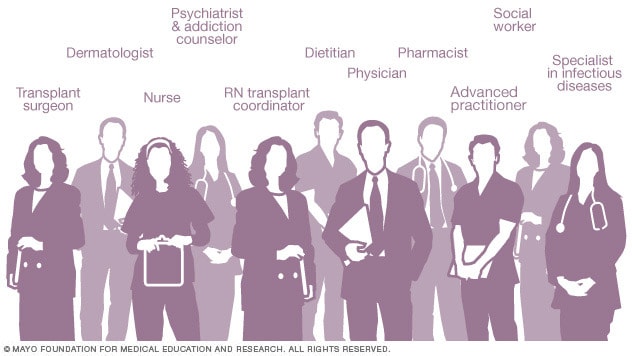
At Mayo Clinic, an integrated team of doctors trained in endocrinology (endocrinologists), abdominal transplant surgery, infectious disease management and other specialties is focused on your needs and the needs of your family before, during and after your pancreas transplant.
Surgeons, doctors, transplant nurses, pharmacists, social workers and others work together to manage every aspect of your pancreas transplant, from planning through post-surgical care.
Coordinated care
 Care team roles
Care team roles
Health care professionals trained in many medical specialties work together as a team to ensure favorable outcomes from your pancreas transplant.
Having all of this subspecialized expertise in a single place, focused on you, means that you're not getting just one opinion — your care is discussed among the team, your test results are available quickly, appointments are scheduled in coordination, and your transplant care team works together to determine what's best for you.
Surgical expertise
Mayo Clinic surgeons have performed hundreds of successful pancreas transplants using state-of-the-art technology since 1987.
Mayo Clinic is one of only a few transplant centers that offer pancreas transplants to select candidates with type 2 diabetes and treated HIV.
Pancreas transplant surgery is provided to children at Mayo Clinic's campus in Rochester, Minnesota.
Research
At Mayo Clinic, you may have access to clinical trials, research studies and new treatments as part of your care.
Researchers in the Mayo Clinic Transplant Center are actively engaged in developing new technologies, treatments and techniques to make transplants safer and available to more people.
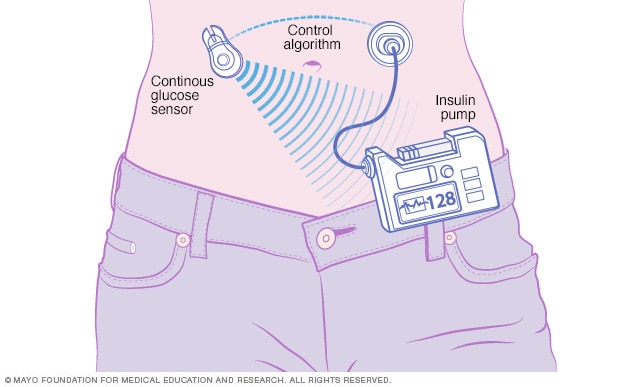
For example, researchers at Mayo Clinic are developing an artificial pancreas that could significantly improve the quality of life for people with type 1 diabetes and potentially provide an alternative to pancreas transplant.
Mayo Clinic researchers are also investigating ways to lower the rejection risk among transplant recipients and seeking new ways to treat people who need transplants of all types.
Read more about the Pancreas Transplant Program at Mayo Clinic.
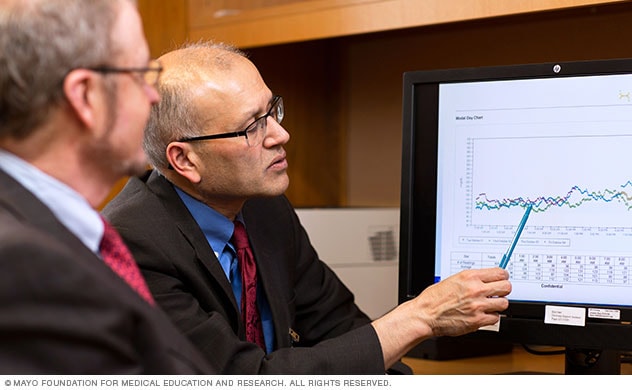
Lowering rejection in organ transplant
Watch Mark Stegall, M.D., and Richard Daly, M.D., discuss lowering rejection risk in organ transplants.
Expertise and rankings
Experience
 Pancreas transplant teamwork at Mayo Clinic
Pancreas transplant teamwork at Mayo Clinic
Mayo Clinic has one of the largest transplant practices in the United States. Across its three sites in Minnesota, Florida and Arizona, Mayo Clinic has performed hundreds of successful pancreas transplants. Each year, about 45 people receive pancreas transplants at Mayo Clinic.
Mayo Clinic is one of only a few transplant centers that offers pancreas transplants to select candidates with type 2 diabetes and treated HIV.
Pancreas transplant outcomes at Mayo Clinic compare favorably with the national average.
Innovation and research
Artificial pancreas
Artificial pancreas
Illustration of artificial pancreas under development at Mayo Clinic
Mayo Clinic surgeons have extensive expertise in many areas of pancreas transplantation, including pancreas-only, simultaneous pancreas-kidney and pancreas-after-kidney transplant.
The Mayo Clinic Transplant Center supports many studies and pancreas transplant research. Mayo Clinic doctors actively research pancreas transplantation techniques and treatment options, presenting their work at national and international meetings.
 Artificial Pancreas Lab
Artificial Pancreas Lab
For example, researchers at Mayo Clinic are developing an artificial pancreas that could significantly improve the quality of life for people with type 1 diabetes and potentially provide an alternative to pancreas transplant.
Mayo Clinic researchers are also investigating ways to lower the rejection risk among transplant recipients and seeking new ways to treat people who need transplants of all types.
Nationally recognized expertise
Mayo Clinic in Rochester, Minnesota, ranks No. 1 for diabetes and endocrinology in the U.S. News & World Report Best Hospitals rankings. Mayo Clinic in Phoenix/Scottsdale, Arizona, and Mayo Clinic in Jacksonville, Florida, are ranked among the Best Hospitals for diabetes and endocrinology by U.S. News & World Report.
Read more about the Pancreas Transplant Program at Mayo Clinic.
Volumes and outcomes
Mayo Clinic's experienced doctors and integrated team approach result in transplant outcomes that compare favorably with national averages. Teams work with transplant recipients before, during and after surgery to ensure the greatest likelihood of superior results.
Volumes and statistics are maintained separately for the three Mayo Clinic locations. Taken together or separately, Mayo Clinic's transplant results are excellent.
Pancreas transplant volumes and statistics
Locations, travel and lodging
Mayo Clinic has major campuses in Phoenix and Scottsdale, Arizona; Jacksonville, Florida; and Rochester, Minnesota. The Mayo Clinic Health System has dozens of locations in several states.
For more information on visiting Mayo Clinic, choose your location below:
Costs and insurance
Mayo Clinic has dedicated transplant financial services representatives and social workers who can assist you with insurance and financial questions regarding your pancreas transplant.
Mayo Clinic works with hundreds of insurance companies and is an in-network provider for millions of people. In most cases, Mayo Clinic doesn't require a physician referral. Some insurers require referrals or may have additional requirements for certain medical care. Many insurance companies require you to get preapproval authorization prior to transplant services.
Read more about pancreas transplant costs and insurance at Mayo Clinic.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Jan. 19, 2024