Overview
Breast augmentation — also known as augmentation mammoplasty — is surgery to increase breast size. It involves placing breast implants under breast tissue or chest muscles.
For some women, breast augmentation is a way to feel more confident. For others, it's part of rebuilding the breast for various conditions.
If you're considering breast augmentation, talk to a plastic surgeon. Make sure you understand what surgery involves, including possible risks, complications and follow-up care.
Products & Services
Why it's done
Breast augmentation might help you:
- Enhance your appearance if you think your breasts are small or that one is smaller than the other and this impacts how you dress or the type of bra needed to help with the asymmetry
- Adjust for a reduction in the size of your breasts after pregnancy or significant weight loss
- Correct uneven breasts after breast surgery for other conditions
- Improve your self-confidence
Discuss your goals with your plastic surgeon so that you can be realistic about what breast augmentation can do for you.
Risks
Breast augmentation poses various risks, including:
- Scar tissue that distorts the shape of the breast implant (capsular contracture)
- Breast pain
- Infection
- Changes in nipple and breast sensation
- Implant position changes
- Implant leakage or rupture
Correcting these complications might require more surgery, to either remove or replace the implants.
Breast implant-associated anaplastic large cell lymphoma
The U.S. Food and Drug Administration (FDA) has identified a possible association between breast implants and the development of anaplastic large cell lymphoma (ALCL), an uncommon cancer of the immune system. The condition is known as breast implant-associated anaplastic large cell lymphoma (BIA-ALCL). The FDA believes that women with breast implants that have textured surfaces have a very low but increased risk of developing BIA-ALCL. However, that doesn't mean that these implants cause BIA-ALCL. Further research is needed to understand the relationship between the condition and breast implants.
Breast implant illness
Systemic symptoms — sometimes called breast implant illness — may be associated with breast implants. The exact relationship of these symptoms to breast implants is not clearly understood. Reported signs and symptoms include fatigue, memory loss, skin rash, trouble concentrating and thinking clearly, and joint pain. Removal of the breast implants may reverse the symptoms. Research to determine the link and the cause is ongoing. Talk to your plastic surgeon if you have breast implants and experience any of these signs and symptoms.
If you notice any changes to your breasts or implants, talk to your doctor. Ongoing follow-up visits and appropriate screening tests can detect and address possible complications related to breast augmentation surgery.
How you prepare
You'll consult with a plastic surgeon about your preferences for size, feel and appearance of your breasts. The surgeon will describe specific types of implants — smooth or textured, round or shaped like a teardrop, saline or silicone — as well as options for surgical techniques.
Carefully review written information, such as the patient information from the manufacturer of the implant you'll be getting, and keep copies for your records.
Before you decide to have surgery, consider the following:
- Breast implants won't prevent your breasts from sagging. Your plastic surgeon may recommend a breast lift in addition to breast augmentation to correct sagging breasts.
- Breast implants aren't guaranteed to last a lifetime. The average life span of an implant is about 10 years. Implant rupture is a possibility. Also, your breasts will continue to age, and factors such as weight gain or weight loss might change the way your breasts look. These issues will likely lead to more surgery.
- Mammograms might be more complicated. If you have breast implants, in addition to routine mammograms, you'll need additional, specialized views.
- Breast implants might hamper breast-feeding. Some women are able to successfully breast-feed after breast augmentation. For others, however, breast-feeding is a challenge.
- Insurance doesn't cover breast implants. Unless it's medically necessary — such as after a mastectomy for breast cancer — breast augmentation isn't covered by insurance. Be prepared to handle the expenses, including related surgeries or future imaging tests.
- You might need additional surgery after breast implant removal. If you decide to have your implants removed, you might need a breast lift or other corrective surgery to help restore your breasts' appearance.
- Screening for silicone implant rupture is recommended. The FDA recommends routine monitoring with a breast MRI five to six years after placement to screen for silicone breast implant rupture. Then, a breast MRI is recommended every two to three years. An ultrasound may be an alternative screening method — unless you have symptoms. Talk to your plastic surgeon about the specific type of imaging needed for routine monitoring of your implants.
You might need a baseline mammogram before your surgery. Your doctor might adjust certain medications before the surgery as well. For example, it's important to avoid aspirin or other medications that can increase bleeding.
If you smoke, your surgeon will ask you to stop smoking for a time — about four to six weeks — before and after the surgery.
Arrange for someone to drive you home after the surgery and to stay with you for at least the first night.
What you can expect
Breast augmentation incision sites
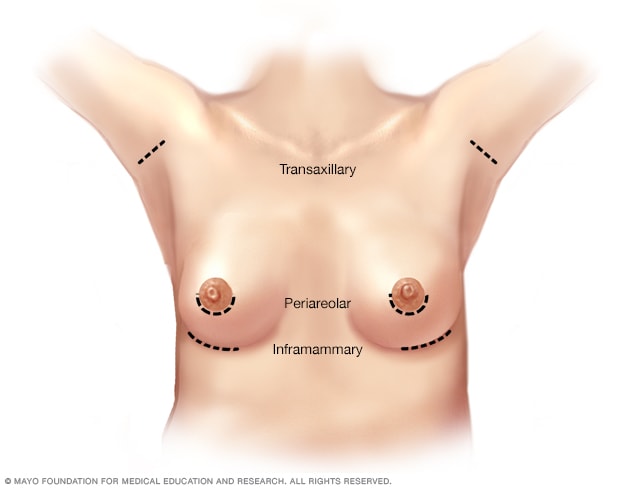
Breast augmentation incision sites
During breast augmentation, the surgeon makes an incision in one of three possible places: the crease under your breast (inframammary), under your arm (axillary) or around your nipple (periareolar).
Placement of breast implants
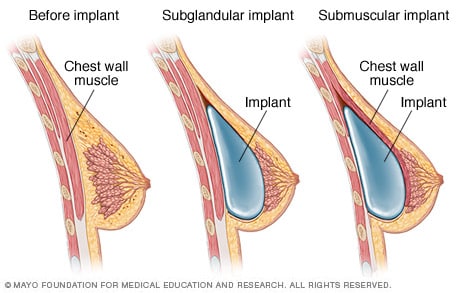
Placement of breast implants
After breast augmentation surgery, the implant lies either behind the glandular tissue in your breast (subglandular placement) or behind the chest wall muscle (submuscular placement).
Breast augmentation can be done in a surgical center or hospital outpatient facility. You'll probably go home the same day. The procedure rarely requires a hospital stay.
Sometimes, breast augmentation is done during local anesthesia — you're awake and your breast area is numbed. Often, though, breast augmentation is done during general anesthesia, in which you're asleep for the surgery. Your plastic surgeon will review different anesthesia options with you.
During the procedure
To insert the breast implant, your plastic surgeon will make a single cut (incision) in one of three places:
- The crease under your breast (inframammary)
- Under your arm (axillary)
- Around your nipple (periareolar)
After making an incision, the surgeon will separate your breast tissue from the muscles and connective tissue of your chest. This creates a pocket either behind or in front of the outermost muscle of the chest wall (pectoral muscle). The surgeon will insert the implant into this pocket and center it behind your nipple.
Saline implants are inserted empty and then filled with sterile salt water once they're in place. Silicone implants are pre-filled with silicone gel.
When the implant is in place, the surgeon will close the incision — typically with stitches (sutures) — and bandage it with skin adhesive and surgical tape.
After the procedure
Soreness and swelling are likely for a few weeks after surgery. Bruising is possible, too. Expect scars to fade over time but not disappear completely.
While you're healing, it might help to wear a compression bandage or sports bra for extra support and positioning of the breast implants. Your surgeon might prescribe pain medication as well.
Follow your surgeon's instructions about returning to regular activities. If you don't have a physically demanding job, you might be able to return to work within a few weeks. Avoid strenuous activities — anything that could raise your pulse or blood pressure — for at least two weeks. While you're healing, remember that your breasts will be sensitive to physical contact or jarring movements.
If your surgeon used sutures that don't absorb on their own or placed drainage tubes near your breasts, you'll need a follow-up appointment for removal.
If you notice warmth and redness in your breast or you have a fever, you might have an infection. Contact your surgeon as soon as possible. Also contact your surgeon if you have shortness of breath or chest pain.
Results
Breast augmentation can change the size and shape of your breasts. The surgery might improve your body image and self-esteem. But keep your expectations realistic, and don't expect perfection.
Also, your breasts will continue to age after augmentation. Weight gain or weight loss might change the way your breasts look, too. If you become dissatisfied with the appearance of your breasts, you might need more surgery to correct these issues.
Aug. 12, 2022