March 28, 2015
The triad of hypertension, hypokalemia and an aldosterone-producing adenoma (APA) of the adrenal gland was first reported by Jerome W. Conn, M.D., in 1955. The hypertension and hypokalemia in Dr. Conn's first patient were cured by removal of an adrenal adenoma.
William F. Young Jr., M.D., of the Division of Endocrinology, Diabetes, Metabolism and Nutrition at Mayo Clinic's campus in Rochester, Minnesota, says: "Over the past 60 years, three facts have become clear: First, primary aldosteronism (PA) is more common than previously thought, and it affects between 5 and 10 percent of all patients with hypertension. Second, most patients with PA are normokalemic. Third, PA has more than one cause, and most patients with PA have bilateral idiopathic hyperaldosteronism (IHA).
"Unilateral adrenalectomy in patients with APA results in normalization of hypokalemia in all patients, normalization of blood pressure in at least a third of patients and improvement of hypertension in the remaining patients. Whereas, in patients with IHA, unilateral or bilateral adrenalectomy seldom corrects hypertension. Patients with IHA should be treated not surgically but medically with a mineralocorticoid receptor antagonist. Therefore, determining the subtype of PA (APA versus IHA) is critical in directing treatment."
In 1967, selective adrenal venous sampling (AVS) for aldosterone was first proposed as a test to distinguish between APA and IHA. However, it is an invasive and difficult technique. The right adrenal vein is small and may be difficult to identify, to cannulate and to withdraw blood from. Both adrenal veins must be sampled for meaningful comparison.
Scan of man with hypokalemia and poorly controlled hypertension
Scan of man with hypokalemia and poorly controlled hypertension
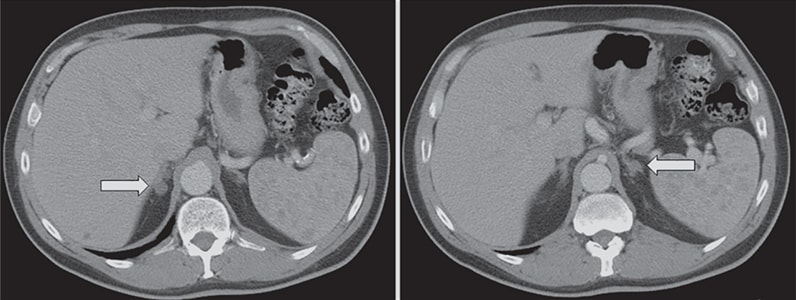
Adrenal computerized tomographic scan of a 59-year-old man with hypokalemia and poorly controlled hypertension despite taking four antihypertensive drugs. The scan shows an 11-mm right adrenal nodule (arrow, left panel) and a 9-mm left adrenal nodule (arrow, right panel). Adrenal venous sampling lateralized aldosterone secretion to the right adrenal gland and a cortical adenoma was found at laparoscopic right adrenalectomy. Following right laparoscopic adrenalectomy, the hypokalemia resolved and his residual hypertension was easily controlled with two antihypertensive medications.
When body computerized tomography (CT) became available in the late 1970s, it was thought to be a good test to distinguish among the subtypes of PA. Dr. Young notes: "However, because of the prevalence of nonfunctioning cortical adenomas, hormonal hyperfunction cannot be inferred from simply the presence of an adrenal nodule. A patient with IHA may be thought to have an APA because an adrenal nodule was detected on CT — a finding that may be due to the age-related occurrence of nonfunctioning adrenal cortical nodules. Yet, APAs that are 3 or 4 mm in diameter may escape detection on CT or a patient with a unilateral APA may have bilateral adrenal nodules on CT — one that is nonfunctional and one that is hypersecreting aldosterone.
Algorithmic approach to subtype evaluation

Algorithmic approach to subtype evaluation
An algorithmic approach to subtype evaluation of a patient with primary aldosteronism. Terms in the chart: aldosterone-producing adenoma (APA); adrenal venous sampling (AVS); computerized tomography (CT); glucocorticoid remediable aldosteronism (GRA); idiopathic hyperaldosteronism (IHA); unilateral adrenal hyperplasia (UAH).
"An approach to these clinical dilemmas is shown in the algorithm, which outlines that AVS is not needed in all patients with PA. Because adrenal 'incidentalomas' are uncommon in young patients, when a solitary unilateral macronodule (greater than 1 cm) and a normal contralateral adrenal are found on CT in a patient with PA who is less than 35 years of age, unilateral adrenalectomy is reasonable to consider.
"In addition, some patients prefer pharmacological therapy over a surgical procedure and therefore AVS is not needed. With this approach, AVS is performed in approximately 25 percent of Mayo Clinic patients with PA."
Patients with an APA have more severe hypertension, more frequent hypokalemia, and higher plasma (greater than 25 ng/dL) and urinary (greater than 30 μg/24 h) levels of aldosterone than do patients with IHA. Patients with these findings are considered to have a "high probability" of APA. However, these findings are not absolute predictors of unilateral versus bilateral adrenal disease.
Adrenal venous sampling
Adrenal venous sampling
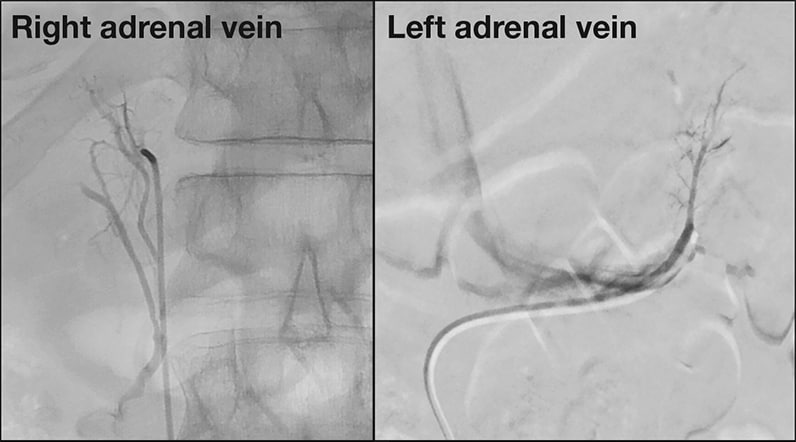
Images of adrenal venous sampling performed in a 59-year-old patient with primary aldosteronism. Radiographs show catheters placed in the right and left adrenal veins.
James C. Andrews, M.D., of the Department of Radiology at Mayo Clinic's campus in Rochester, Minnesota, says: "We have now performed AVS in more than 700 patients. The adrenal veins are sequentially catheterized through the percutaneous femoral vein approach under fluoroscopic guidance, and correct catheter tip location is confirmed with injection of a small amount of contrast medium. Blood is obtained by gentle aspiration from both adrenal veins. Successful catheterization may require an array of catheter configurations, either available from manufacturers or custom made with steam shaping during the procedure to facilitate access to the adrenal veins.
Results of bilateral adrenal venous sampling

Results of bilateral adrenal venous sampling
Results of bilateral adrenal venous sampling performed in a 59-year-old patient with primary aldosteronism. The cortisol concentrations from the adrenal veins and inferior vena cava are used to confirm successful catheterization; the adrenal vein cortisol-to-inferior vena cava cortisol ratio is typically more than 10-to-1 when the protocol for continuous cosyntropin infusion is followed (minimum cutoff is greater than a ratio of 5-to-1). Dividing the plasma aldosterone concentrations (PACs) of the right and left adrenal veins by the respective cortisol concentrations corrects for the dilutional effect of blood from the inferior phrenic vein flowing into the left adrenal vein; these quotients are termed cortisol-corrected aldosterone ratios. In patients with aldosterone-producing adenoma (APA), the mean cortisol-corrected aldosterone ratio (APA-side PAC/cortisol concentration-to-normal adrenal PAC/cortisol concentration ratio) is 18-to-1. A cutoff for the cortisol-corrected aldosterone ratio from high side to low side of more than 4-to-1 is used to indicate unilateral aldosterone excess. The lateralizaton ratio in this patient is 6.2-to-1 and is consistent with a right adrenal APA.
"At centers with experience with AVS, the complication rate is 2.5 percent or less. Complications can include symptomatic groin hematoma, adrenal hemorrhage and dissection of an adrenal vein. Aldosterone and cortisol concentrations are measured in the blood from all three sites: right adrenal vein, left adrenal vein and IVC. All of the blood samples should be assayed at ratios of 1-to-1, 1-to-10 and 1-to-50 dilutions — absolute values are mandatory. Accurate laboratory assays for cortisol and aldosterone are keys to successful interpretation of the AVS data."
Dr. Young concludes: "For patients with PA who want to pursue the surgical treatment option, AVS is the key diagnostic step."