Overview
Wolff-Parkinson-White (WPW) syndrome
Wolff-Parkinson-White (WPW) syndrome
In Wolff-Parkinson-White (WPW) syndrome, an extra electrical pathway between the heart's upper chambers and lower chambers causes a fast heartbeat.
Wolff-Parkinson-White (WPW) syndrome is a heart condition present at birth. That means it's a congenital heart defect. People with WPW syndrome have an extra pathway for signals to travel between the heart's upper and lower chambers. This causes a fast heartbeat. Changes in the heartbeat can make it harder for the heart to work as it should.
WPW syndrome is fairly rare. Another name for it is preexcitation syndrome.
The episodes of fast heartbeats seen in Wolff-Parkinson-White syndrome usually aren't life-threatening. But serious heart problems can occur. Rarely, the syndrome may lead to sudden cardiac death in children and young adults.
Treatment of WPW syndrome may include special actions, medicines, a shock to the heart or a procedure to stop the irregular heartbeats.
Products & Services
Symptoms
The heart rate is the number of times the heart beats each minute. A fast heart rate is called tachycardia (tak-ih-KAHR-dee-uh).
The most common symptom of Wolff-Parkinson-White (WPW) syndrome is a heart rate greater than 100 beats a minute.
In WPW syndrome, the fast heartbeat can begin suddenly. It may last a few seconds or several hours. Episodes may occur during exercise or while at rest.
Other symptoms of WPW syndrome may depend on the speed of the heartbeat and the underlying heart rhythm disorder.
For example, the most common irregular heartbeat seen with WPW syndrome is supraventricular tachycardia (SVT). During an episode of SVT, the heart beats about 150 to 220 times a minute, but it can occasionally beat faster or slower.
Some people with WPW syndrome also have a fast and chaotic heart rhythm disorder called atrial fibrillation.
In general, symptoms of WPW syndrome include:
- Rapid, fluttering or pounding heartbeats.
- Chest pain.
- Difficulty breathing.
- Dizziness or lightheadedness.
- Fainting.
- Fatigue.
- Shortness of breath.
- Anxiety.
Symptoms in infants
Infants with WPW may have other symptoms, such as:
- Blue or gray skin, lips and nails. These changes may be harder or easier to see depending on skin color.
- Restlessness or irritability.
- Rapid breathing.
- Poor eating.
Some people with an extra electrical pathway don't have symptoms of a fast heartbeat. This condition is called Wolff-Parkinson-White (WPW) pattern. It's often discovered by chance during a heart test.
When to see a doctor
Many things can cause a fast heartbeat. It's important to get a prompt diagnosis and care. Sometimes a fast heartbeat isn't a concern. For example, the speed of the heartbeat may increase with exercise.
If you feel like your heart is beating too fast, make an appointment to see a healthcare professional.
Call 911 or your local emergency number if you have any of the following symptoms for more than a few minutes:
- Sensation of a fast or pounding heartbeat.
- Difficulty breathing.
- Chest pain.
Causes
Typical heartbeat
Typical heartbeat
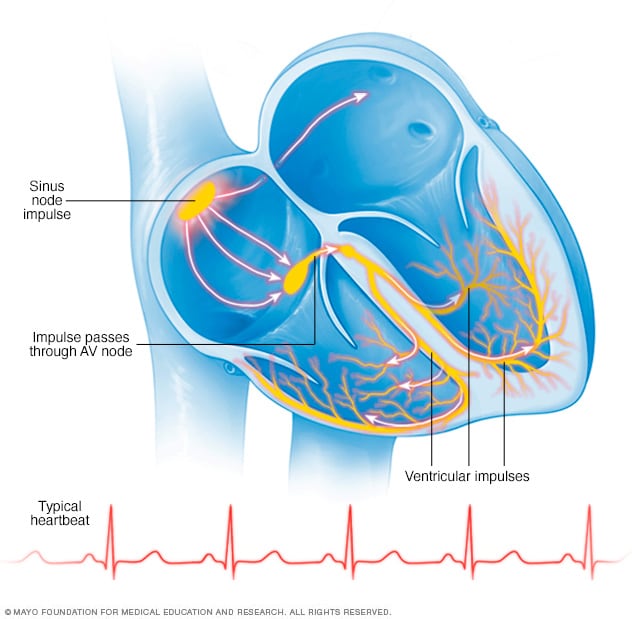
In a typical heart rhythm, a tiny cluster of cells at the sinus node sends out an electrical signal. The signal then travels through the atria to the atrioventricular (AV) node and then passes into the ventricles, causing them to contract and pump out blood.
Wolff-Parkinson-White (WPW) syndrome is a heart condition present at birth. That means it's a congenital heart defect. Researchers aren't sure what causes most types of congenital heart defects. WPW syndrome may occur with other congenital heart defects, such as Ebstein anomaly.
Rarely, WPW syndrome is passed down through families. Your healthcare team may call this inherited or familial WPW syndrome. It is associated with a thickened heart muscle, called hypertrophic cardiomyopathy.
To understand the causes of WPW syndrome, it may be helpful to know how the heart typically beats.
The heart has four chambers.
- The two upper chambers are called the atria.
- The two lower chambers are called the ventricles.
Inside the upper right heart chamber is a group of cells called the sinus node. The sinus node makes the signals that start each heartbeat.
The signals move across the upper heart chambers. Next, the signals arrive at a group of cells called the atrioventricular (AV) node, where they usually slow down. The signals then go to the lower heart chambers.
In a typical heart, this signaling process usually goes smoothly. The resting heart rate is about 60 to 100 beats a minute.
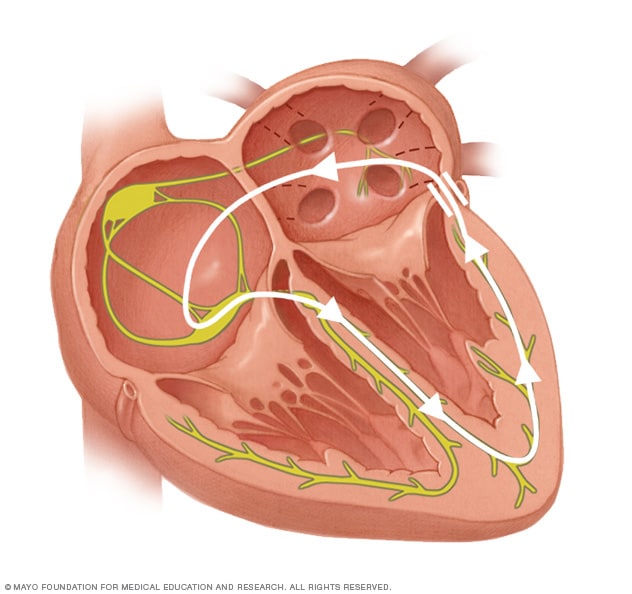
In WPW syndrome, an extra electrical pathway connects the upper and lower heart chambers, allowing heart signals to bypass the AV node. As a result, the heart signals don't slow down. The signals get excited, and the heart rate gets faster. The extra pathway also can cause heart signals to travel backward. This causes an uncoordinated heart rhythm.
Complications
WPW syndrome has been linked to sudden cardiac death in children and young adults.
Dec. 13, 2023