Overview
Varicose veins
Varicose veins
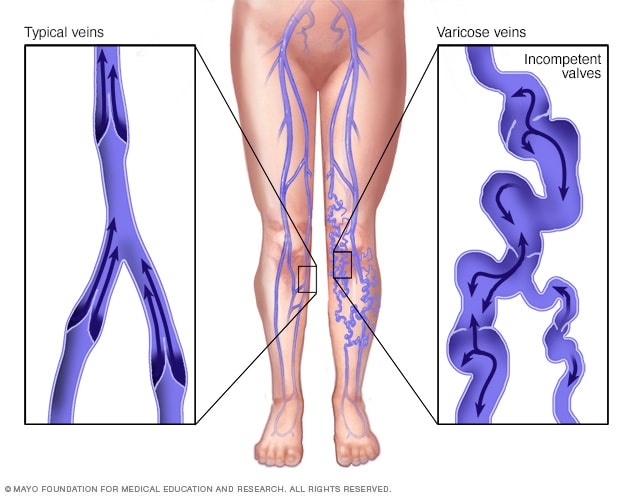
Veins return blood from the rest of the body to the heart. To return blood to the heart, the veins in the legs must work against gravity. Weakened valves, also called incompetent valves, within the veins might cause varicose veins. The weakened valves let blood pool in the veins instead of traveling to the heart. When blood pools in the veins, the veins become larger, making them show under the skin.
Varicose veins are bulging, enlarged veins. Any vein that is close to the skin's surface, called superficial, can become varicosed. Varicose veins most often affect the veins in the legs. That's because standing and walking increase the pressure in the veins of the lower body.
For many people, varicose veins are simply a cosmetic concern. So are spider veins, a common, mild form of varicose veins. But varicose veins can cause aching pain and discomfort. Sometimes they lead to more-serious health problems.
Treatment involves exercising, raising legs when sitting or lying down, or wearing compression stockings. A procedure may be done to close or remove veins.
Products & Services
Symptoms
Spider veins

Spider veins
Spider veins appear as thin, red lines or as weblike networks of blood vessels on the surface of the skin. Spider veins, a mild form of varicose veins, most often appear on the legs and feet.
Varicose veins might not cause pain. Symptoms of varicose veins include:
- Veins that are dark purple, blue or the same color as the skin. Depending on skin color, these changes may be harder or easier to see.
- Veins that look twisted and bulging. They often look like cords on the legs.
When there are painful symptoms of varicose veins, they might include:
- An achy or heavy feeling in the legs.
- Burning, throbbing, muscle cramping and swelling in the lower legs.
- Worse pain after sitting or standing for a long time.
- Itching around one or more of the veins.
- Changes in skin color around a varicose vein.
Spider veins are like varicose veins, but they're smaller. Spider veins are found closer to the skin's surface and might look like a spider's web.
Spider veins occur on the legs but also can be found on the face. They vary in size and often look like a spider's web.
When to see a doctor
If you worry about how your veins look and feel and self-care measures haven't helped, see your healthcare professional.
Causes
Weak or damaged valves can lead to varicose veins. Arteries carry blood from the heart to the rest of the body. Veins return blood from the rest of the body to the heart. To return blood to the heart, the veins in the legs must work against gravity.
Muscles tighten in the lower legs to act as pumps. Vein walls help blood return to the heart. Tiny valves in the veins open as blood flows toward the heart, then close to stop blood from flowing backward. If these valves are weak or damaged, blood can flow backward and pool in the veins, causing the veins to stretch or twist.
Risk factors
The two main risk factors for varicose veins are:
- Family history. If other family members have varicose veins, there's a greater chance you will too.
- Obesity. Being overweight puts added pressure on veins.
Other things that might increase the risk of varicose veins include:
- Age. Aging causes wear and tear on the valves in the veins that help control blood flow. Over time, that wear causes the valves to allow some blood to flow back into the veins, where it collects.
- Sex. Women are more likely to get the condition. Hormones tend to relax vein walls. So changes in hormones before a menstrual period or during pregnancy or menopause might be a factor. Hormone treatments, such as birth control pills, might increase the risk of varicose veins.
- Pregnancy. During pregnancy, the blood volume in the body increases. This change supports the growing baby but also can make the veins in the legs bigger.
- Standing or sitting for long periods of time. Movement helps blood flow.
Complications
Complications of varicose veins are rare. They can include:
- Ulcers. Painful ulcers can form on the skin near varicose veins, mostly near the ankles. A discolored spot on the skin often begins before an ulcer forms. See your healthcare professional right away if you think you have a leg ulcer.
- Blood clots. Sometimes, veins deep within the legs get larger. They might cause leg pain and swelling. Seek medical help for ongoing leg pain or swelling. This can mean a blood clot.
- Bleeding. Rarely, veins close to the skin burst. This mostly causes only minor bleeding. But it needs medical help.
- Leg swelling. Longtime varicose veins can cause the legs to swell.
Prevention
Getting better blood flow and muscle tone might lower the risk of having varicose veins. The same ways you treat the discomfort from varicose veins can help prevent them. Try the following:
- Don't wear high heels or tight stockings, other than compression stockings.
- Change how you sit or stand often.
- Eat a high-fiber, low-salt diet.
- Exercise.
- Raise your legs when sitting or lying down.
- Keep a healthy weight.
Feb. 06, 2024