Diagnosis
Health care professionals often can figure out if someone has Peyronie disease by doing a physical exam. They also might do tests to check for other conditions that can cause similar symptoms.
You might need the following tests:
-
Physical exam. Your health care professional feels your penis when it's not erect to figure out the location and amount of scar tissue. The length of your penis also might be measured. If the condition becomes worse, this measurement helps determine whether the penis has gotten shorter.
Your health care professional also might ask you to bring in photos of your erect penis taken at home. This can help determine the degree of curving, the location of scar tissue or other details that might guide treatment.
-
Other tests. Your health care professional might order an ultrasound or other tests to check your penis when it's erect. Before testing, you'll likely receive a shot directly into the penis that helps it become erect.
Ultrasound is the most commonly used test for penis conditions. It uses sound waves to make images of soft tissues inside the body. These tests can show the presence of scar tissue, blood flow to the penis and any other irregular signs.
Treatment
Treatment options for Peyronie disease depend on how long it's been since you began having symptoms.
- Acute phase. As scar tissue forms, changes in the curve or length of the penis become worse. You also may have pain during erections. The acute phase may last for 5 to 18 months.
- Chronic phase. The scar tissue in the penis stops growing, and your symptoms become stable. You also have no penile pain or changes in the curve, length or other aspects of the penis. The chronic phase happens later in Peyronie disease.
Acute phase Peyronie disease treatment
For the acute phase of the condition, treatments include:
- Traction therapy. When used early in the process, a device that holds the penis in a cradle and applies tension can be helpful. This is called penile traction therapy. It prevents length loss and limits curving.
- Medicines. Some medicines taken by mouth or given in shots are options in this phase. Some medicines that have been used in the past clearly do not work. Others may or may not help. Your health care professional will likely talk with you in more detail.
Surgery is not recommended in the acute phase of Peyronie disease. It isn't a treatment option until the condition stops becoming worse and any pain goes away. This lowers the chances of needing a second surgery.
Chronic phase Peyronie disease treatment
For the chronic phase of the disease, treatment choices include:
- Watchful waiting, in which your health care team watches your condition closely and gives treatment if your symptoms become worse.
- Injections or shots into the scar tissue.
- Stretching devices, also called "traction" therapy.
- Surgery to straighten the penis.
These treatments may be done alone or combined with one another.
Oral medications taken by mouth aren't recommended in the chronic phase. They haven't been shown to be effective at this stage of the disease.
Medications
Oral medicines have been tried to treat Peyronie disease. But research has shown that many don't work consistently, and they are not as effective as other treatments.
In some people, medicines injected directly into the scar tissue on the penis might reduce curving and pain linked with Peyronie disease. Depending on the treatment, you might be given medicine that goes on the skin called a local anesthetic to prevent pain during the shots.
If you have one of these treatments, you'll likely receive more than one shot over many months. Injection medicines also may be used along with oral medicines or traction therapy.
Medicines given by injection include:
-
Collagenase clostridium histolyticum (Xiaflex). This is the only FDA-approved medicine for Peyronie disease. It's approved for use in adults with a moderate to severe curve and lumps under the skin that can be felt.
This treatment has been shown to improve curving and bothersome symptoms linked with Peyronie disease. The treatment works by breaking down the buildup of collagen protein in the scar tissue that causes the penis to curve. Collagenase seems to work better when it's used along with traction therapy or another treatment called "modeling." With modeling, a health care professional bends the penis in the opposite direction of the curve.
- Verapamil. This medicine appears to work by disrupting the scar tissue and preventing further scar tissue from forming. It may help improve pain too. Verapamil also is used to treat high blood pressure.
- Interferon. This medicine seems to disrupt fibrous tissue from being made. Interferon also seems to help break the fibrous tissue down. Interferon also has been shown to ease penile pain in people with Peyronie disease.
Ask your health care professional about the side effects of any medicine that you might take.
Traction therapy
Penile traction therapy
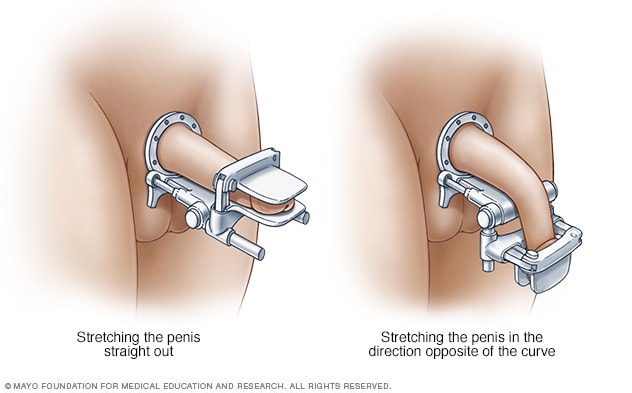
Penile traction therapy
With penile traction therapy, you wear a penile traction device for a set amount of time each day. The device may stretch the penis straight out, or it may stretch the penis in the direction that's opposite of the curve.
Penile traction therapy involves stretching the penis with a mechanical device that you put on daily. You stretch your penis for a set amount of time to improve the length, curve and any other physical changes.
Depending on the specific device, traction therapy may need to be worn for as little as 30 minutes. Or it may need to be worn for as much as 3 to 8 hours a day. How well the treatment works also may depend on the specific device used.
Traction therapy is recommended in the early phase of Peyronie disease. It's the only treatment shown to improve penis length. Traction therapy also may be used in the chronic phase of the disease, combined with other treatments or after surgery for a better outcome.
Surgery
Plication of the penis
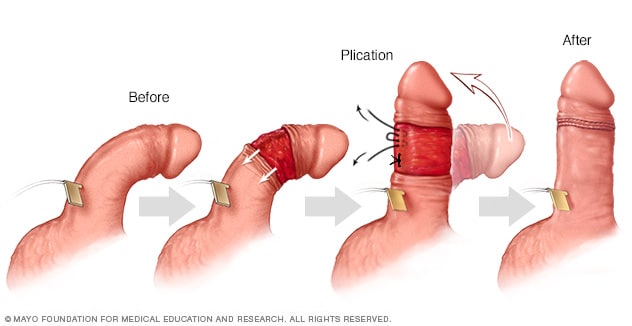
Plication of the penis
During plication of the penis, an artificial erection is created from either injection of a saltwater solution or selected medications. The outer skin of the penis is pulled back. The penis is straightened, and the excess tissue on what had been the outer side of the curve is cinched together by placing a series of stitches or "tucks." The final penile length will depend on the length of the shorter side — the side with the scarring from Peyronie disease.
Graft repair of the penis
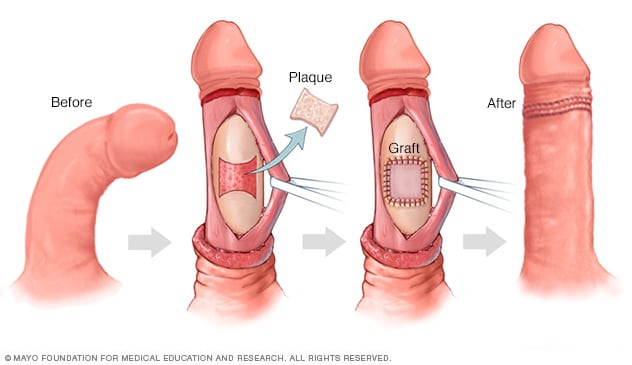
Graft repair of the penis
During a graft repair procedure, your surgeon makes one or more cuts in the scar tissue, also called plaque, of the penis. This allows the sheath to stretch out and the penis to straighten. A patch made of human or animal tissue or a synthetic material is placed to cover the area where scar tissue was removed.
Your doctor might suggest surgery if the curve or bend of your penis is severe, bothers you a lot or prevents you from having sex. Most often, surgery isn't recommended until you've had Peyronie disease for 9 to 12 months. It's also not recommended until the curve of your penis stops getting worse and stays the same for at least 3 to 6 months, and any pain goes away.
Common types of surgery for Peyronie disease include:
-
Suturing the unaffected side. Various procedures can be used to straighten the penis by restricting the longer side without scar tissue. These techniques are called suturing or plicating. They're often used only for curves that are less severe.
Many plication techniques may be used. Most often, they have similar success rates. But the success of the surgery also depends on the surgeon's experience and preference.
-
Incision or excision and grafting. With this type of surgery, the surgeon makes one or more cuts in the scar tissue. This lets the sheath stretch out and the penis straighten. The surgeon might remove some of the scar tissue.
A piece of tissue called a graft often is sewn into place to cover the holes in the tunica albuginea. The graft might be tissue from your own body, human or animal tissue.
Most often, this procedure is used to treat a serious curvature or other change, such as dents in the penis.
-
Penile implants. Surgery is done to place a device into the spongy tissue that fills with blood during an erection. You might receive implants that you can bend down most of the time and bend upward for sex. These are called semirigid implants.
More often, another type of implant is inflated with a pump implanted in the scrotum. Penile implants might be considered if you have both Peyronie disease and erectile dysfunction.
When the implants are put in place, the surgeon might do other procedures to improve the curve in the penis if needed.
The type of surgery used depends on your condition. Your health care team likely will take into account where in the penis your scar tissue is, how serious your symptoms are and other factors. If you are not circumcised, your health care professional might recommend a circumcision during surgery.
Depending on the type of surgery you have, you might be able to go home from the hospital the same day. Or you might need to stay overnight. Your surgeon lets you know how long you should wait before you go back to work. Most often, you take a few days off. After surgery for Peyronie disease, you'll need to wait 4 to 8 weeks before any sexual activity.
Before you get surgery for Peyronie disease, ask your surgeon about the risks. These may include:
- Loss of feeling in the penis.
- Erectile dysfunction.
- More shortening of the penis.
- Infection.
- Rarely, the return of a curve in the penis after surgery.
Other treatments
A technique known as iontophoresis uses an electric current to deliver verapamil along with a steroid through the skin. Research has shown mixed results on improvement in curving of the penis and erectile function.
Researchers continue to explore other treatments for Peyronie disease. Evidence is limited on how well they work and what their side effects might be. Examples include use of intense sound waves to break up scar tissue, stem cells, platelet-rich plasma and radiation therapy. Currently, these therapies are considered experimental.
Our caring team of Mayo Clinic experts can help you with your health concerns. Visit Mayo Clinic Men's Health to
get started.
Get the process started
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Coping and support
Peyronie disease can cause anxiety and create stress between you and your sexual partner.
These tips might help you better cope with Peyronie disease:
- Explain to your partner what the disease is and how it affects your ability to have sex.
- Let your partner know how you feel about the appearance of your penis and your ability to have sex.
- Talk to your partner about how the two of you can maintain sexual and physical closeness.
- Talk to a mental health professional who is skilled in family relations and sexual matters.
Preparing for your appointment
If you have Peyronie disease symptoms, you're likely to start by seeing your family doctor or general practitioner. You might be referred to a specialist in male sexual disorders called a urologist. Encourage your partner to join you at the checkup.
Preparing for your appointment will help you make the best use of your time.
What you can do
Make a list ahead of time that you can share with your health care professional. Your list should include:
- Symptoms you've had, including any that might not seem related to Peyronie disease.
- Key personal information, including any major stresses or recent life changes.
- Medicines that you take, including any vitamins or supplements.
- History of injury to the penis.
- Family history of Peyronie disease, if any.
- Questions to ask your health care team.
You might want to ask some of the following questions:
- What tests will I need?
- What treatment do you recommend?
- Can you tell if my symptoms are likely to become worse or get better?
- Are there any brochures or other printed material that I can take home with me? What websites do you recommend?
Feel free to ask any other questions you think of during your appointment.
What to expect from your doctor
Your doctor or other members of your health care team are likely to ask you some questions. Be ready to answer them. That way, you might have time to go over any points you want to talk about more. You might be asked:
- When did you first notice a curve in your penis or scar tissue under the skin of your penis?
- Has the curve in your penis become worse over time?
- Do you have pain during erections? If so, has it gotten worse or improved over time?
- Do you recall having an injury to your penis?
- Do your symptoms limit your ability to have sex?
Your health care professional also might ask you to complete a survey, such as the International Index of Erectile Function. This helps you describe how the condition affects your ability to have sex.
Our caring team of Mayo Clinic experts can help you with your health concerns. Visit Mayo Clinic Men's Health to
get started.
Get the process started