Overview
Ovarian hyperstimulation syndrome is an exaggerated response to excess hormones. It usually occurs in women taking injectable hormone medications to stimulate the development of eggs in the ovaries. Ovarian hyperstimulation syndrome (OHSS) causes the ovaries to swell and become painful.
ovarian hyperstimulation syndrome (OHSS) may occur in women undergoing in vitro fertilization (IVF) or ovulation induction with injectable medications. Less often, OHSS happens during fertility treatments using medications you take by mouth, such as clomiphene.
Treatment depends on the severity of the condition. OHSS may improve on its own in mild cases, while severe cases may require hospitalization and additional treatment.
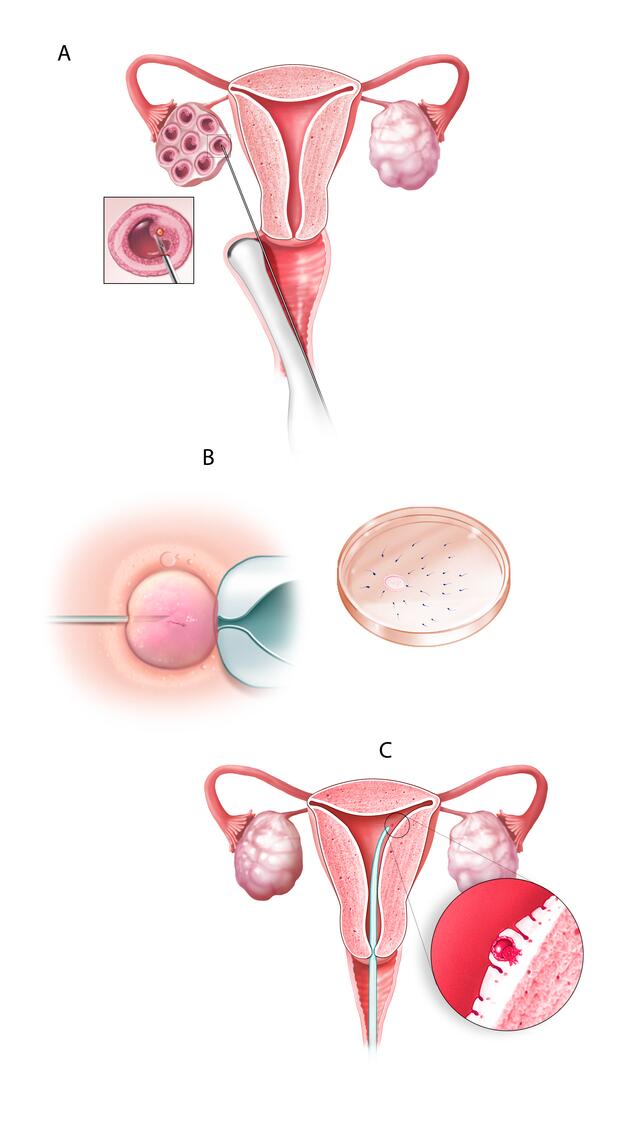
In vitro fertilization
During in vitro fertilization, eggs are removed from mature follicles within an ovary (A). An egg is fertilized by injecting a single sperm into the egg or mixing the egg with sperm in a petri dish (B). The fertilized egg (embryo) is transferred into the uterus (C).
Symptoms
Symptoms of ovarian hyperstimulation syndrome often begin within a week after using injectable medications to stimulate ovulation, though sometimes it can take two weeks or longer for symptoms to appear. Symptoms can range from mild to severe and may worsen or improve over time.
Mild to moderate OHSS
With mild to moderate ovarian hyperstimulation syndrome, symptoms can include:
- Mild to moderate abdominal pain
- Abdominal bloating or increased waist size
- Nausea
- Vomiting
- Diarrhea
- Tenderness in the area of your ovaries
Some women who use injectable fertility drugs get a mild form of OHSS. This usually goes away after about a week. But, if pregnancy occurs, symptoms of OHSS may worsen and last several days to weeks.
Severe OHSS
With severe ovarian hyperstimulation syndrome, you might have:
- Rapid weight gain — more than 2.2 pounds (1 kilogram) in 24 hours
- Severe abdominal pain
- Severe, persistent nausea and vomiting
- Blood clots
- Decreased urination
- Shortness of breath
- Tight or enlarged abdomen
When to see a doctor
If you're having fertility treatments and you experience symptoms of ovarian hyperstimulation syndrome, tell your health care provider. Even if you have a mild case of OHSS, your provider will want to observe you for sudden weight gain or worsening symptoms.
Contact your provider right away if you develop breathing problems or pain in your legs during your fertility treatment. This may indicate an urgent situation that needs prompt medical attention.
Women’s health topics – straight to your inbox
Causes
The cause of ovarian hyperstimulation syndrome isn't fully understood. Having a high level of human chorionic gonadotropin (HCG) — a hormone usually produced during pregnancy — introduced into your system plays a role. Ovarian blood vessels react abnormally to human chorionic gonadotropin (HCG) and begin to leak fluid. This fluid swells the ovaries, and sometimes large amounts move into the abdomen.
During fertility treatments, HCG may be given as a "trigger" so that a mature follicle will release its egg. OHSS usually happens within a week after you receive an HCG injection. If you become pregnant during a treatment cycle, OHSS may worsen as your body begins producing its own HCG in response to the pregnancy.
Injectable fertility medications are more likely to cause OHSS than is treatment with clomiphene, a medication given as a pill you take by mouth. Occasionally OHSS occurs spontaneously, not related to fertility treatments.
Risk factors
Sometimes, OHSS happens in women with no risk factors at all. But factors that are known to increase your risk of OHSS include:
- Polycystic ovary syndrome — a common reproductive disorder that causes irregular menstrual periods, excess hair growth and unusual appearance of the ovaries on ultrasound examination
- Large number of follicles
- Age under 35
- Low body weight
- High or steeply increasing level of estradiol (estrogen) before an HCG trigger shot
- Previous episodes of OHSS
Complications
Severe ovarian hyperstimulation syndrome is uncommon, but can be life-threatening. Complications may include:
- Fluid collection in the abdomen and sometimes the chest
- Electrolyte disturbances (sodium, potassium, others)
- Blood clots in large vessels, usually in the legs
- Kidney failure
- Twisting of an ovary (ovarian torsion)
- Rupture of a cyst in an ovary, which can lead to serious bleeding
- Breathing problems
- Pregnancy loss from miscarriage or termination because of complications
- Rarely, death
Prevention
To decrease your chances of developing ovarian hyperstimulation syndrome, you'll need an individualized plan for your fertility medications. Expect your health care provider to carefully monitor each treatment cycle, including frequent ultrasounds to check the development of follicles and blood tests to check your hormone levels.
Strategies to help prevent OHSS include:
- Adjusting medication. Your provider uses the lowest possible dose of gonadotropins to stimulate your ovaries and trigger ovulation.
- Adding medication. Some medications seem to reduce the risk of OHSS without affecting the odds of pregnancy. These include low-dose aspirin; dopamine agonists such as carbergoline or quinogloide; and calcium infusions. Giving women who have polycystic ovary syndrome the drug metformin (Glumetza) during ovarian stimulation may help prevent hyperstimulation.
- Coasting. If your estrogen level is high or you have a large number of developed follicles, your provider may have you stop injectable medications and wait a few days before giving HCG, which triggers ovulation. This is known as coasting.
- Avoiding use of an HCG trigger shot. Because OHSS often develops after an HCG trigger shot is given, alternatives to HCG for triggering have been developed using gonadotropin-releasing hormone (Gn-RH) agonists, such as leuprolide (Lupron), as a way to prevent or limit OHSS.
- Freezing embryos. If you're undergoing in vitro fertilization (IVF), all the follicles (mature and immature) may be removed from your ovaries to reduce the chance of OHSS. Mature follicles are fertilized and frozen, and your ovaries are allowed to rest. You can resume the IVF process at a later date, when your body is ready.