Diagnosis
Bone marrow exam
Bone marrow exam
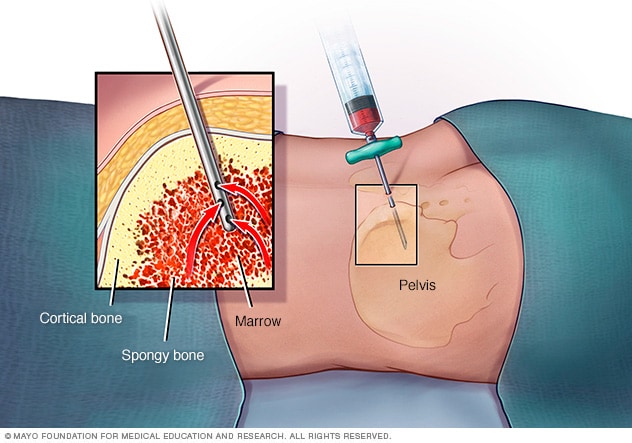
In a bone marrow aspiration, a health care provider uses a thin needle to remove a small amount of liquid bone marrow, usually from a spot in the back of your hipbone (pelvis). A bone marrow biopsy is often done at the same time. This second procedure removes a small piece of bone tissue and the enclosed marrow.
Your doctor will likely ask you about your personal and family medical history. He or she may then have you undergo tests and procedures used to diagnose non-Hodgkin's lymphoma, including:
- Physical exam. Your doctor checks for swollen lymph nodes, including in your neck, underarm and groin, as well as for a swollen spleen or liver.
- Blood and urine tests. Blood and urine tests may help rule out an infection or other disease.
- Imaging tests. Your doctor may recommend imaging tests to look for signs of lymphoma cells elsewhere in your body. Tests may include CT, MRI and positron emission tomography (PET).
- Lymph node test. Your doctor may recommend a lymph node biopsy procedure to remove all or part of a lymph node for laboratory testing. Analyzing lymph node tissue in a lab may reveal whether you have non-Hodgkin's lymphoma and, if so, which type.
- Bone marrow test. A bone marrow biopsy and aspiration procedure involves inserting a needle into your hipbone to remove a sample of bone marrow. The sample is analyzed to look for non-Hodgkin's lymphoma cells.
- Lumbar puncture (spinal tap). If there's a concern that the lymphoma may affect the fluid around your spinal cord, your doctor might recommend a procedure to remove some of the fluid for testing. During a spinal tap, the doctor inserts a small needle into the spinal canal in your lower back.
Other tests and procedures may be used depending on your situation.
Your doctor uses information from these tests and procedures to determine the subtype of your non-Hodgkin's lymphoma and which treatments may be most effective. Many types of non-Hodgkin's lymphoma exist, including rare forms that some doctors may have never seen. Research shows that having your tissue samples reviewed by an experienced doctor may result in a more accurate diagnosis. If you have any concerns about your diagnosis, consider seeking a second opinion.
More Information
Treatment
Several non-Hodgkin's lymphoma treatments are available. Which treatment or combination of treatments is best for you will depend on the particulars of your lymphoma, such as the types of cells involved and whether your lymphoma is aggressive. Your doctor also considers your overall health and your preferences.
If your lymphoma appears to be slow growing (indolent) and doesn't cause signs and symptoms, you might not need treatment right away. Instead, your doctor may recommend regular checkups every few months to monitor your condition and whether your cancer is advancing.
If your non-Hodgkin's lymphoma is aggressive or causes signs and symptoms, your doctor may recommend treatment. Options may include:
Chemotherapy
Chemotherapy is a drug treatment that kills cancer cells. It can be given orally or by injection. Chemotherapy drugs can be used alone, in combination with other chemotherapy drugs or combined with other treatments.
Chemotherapy is a common initial treatment for non-Hodgkin's lymphoma. It might also be an option if your lymphoma comes back after your initial treatments.
For people with non-Hodgkin's lymphoma, chemotherapy is also used as part of a bone marrow transplant, also known as a stem cell transplant. Very high doses of chemotherapy drugs can help prepare your body for the transplant.
Radiation therapy
Radiation therapy uses high-powered energy beams, such as X-rays and protons, to kill cancer cells. During radiation therapy, you lie on a table and a large machine moves around you, directing the energy beams to specific points on your body.
For certain types of non-Hodgkin's lymphoma, radiation therapy may be the only treatment you need, particularly if your lymphoma is slow growing and located in just one or two spots. More commonly, radiation is used after chemotherapy to kill any lymphoma cells that might remain. Radiation can be aimed at affected lymph nodes and the nearby area of nodes where the disease might progress.
Targeted drug therapy
Targeted drug treatments focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die.
For non-Hodgkin's lymphoma, targeted drugs can be used alone, but are often combined with chemotherapy. This combination can be used as your initial treatment and as a second treatment if your lymphoma comes back.
Engineering immune cells to fight lymphoma
A specialized treatment called chimeric antigen receptor (CAR)-T cell therapy takes your body's germ-fighting T cells, engineers them to fight cancer and infuses them back into your body.
CAR-T cell therapy might be an option for certain types of B-cell non-Hodgkin's lymphoma that haven't responded to other treatments.
Bone marrow transplant
Bone marrow transplant, also known as a stem cell transplant, involves using high doses of chemotherapy and radiation to suppress your bone marrow and immune system. Then healthy bone marrow stem cells from your body or from a donor are infused into your blood where they travel to your bones and rebuild your bone marrow.
For people with non-Hodgkin's lymphoma, a bone marrow transplant might be an option if other treatments haven't helped.
Immunotherapy
Immunotherapy uses your immune system to fight cancer. Your body's disease-fighting immune system may not attack your cancer because the cancer cells produce proteins that help them hide from the immune system cells. Immunotherapy works by interfering with that process.
Immunotherapy drugs may be an option for certain types of non-Hodgkin's lymphoma if other treatments haven't helped.
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Alternative medicine
No alternative medicines have been found to cure non-Hodgkin's lymphoma. But alternative medicine may help you cope with the stress of a cancer diagnosis and the side effects of cancer treatment. Talk with your doctor about your options, such as:
- Art therapy
- Exercise
- Meditation
- Music therapy
- Relaxation exercises
- Spirituality
Coping and support
A non-Hodgkin's lymphoma diagnosis can be overwhelming. The following strategies and resources may help you deal with cancer:
- Learn about non-Hodgkin's lymphoma. Learn enough about your cancer to feel comfortable making decisions about your treatment and care. In addition to talking with your doctor, look for information in your local library and on the internet. Start your information search with the National Cancer Institute and the Leukemia & Lymphoma Society.
-
Maintain a strong support system. Keeping your close relationships strong will help you deal with your non-Hodgkin's lymphoma. Friends and family can provide the practical support you'll need, such as helping take care of your house if you're in the hospital. And they can serve as emotional support when you feel overwhelmed by cancer.
Although friends and family can be your best allies, they sometimes may have trouble dealing with your illness. If so, the concern and understanding of a formal support group or others coping with cancer can be especially helpful.
- Set reasonable goals. Having goals helps you feel in control and can give you a sense of purpose. But avoid setting goals you can't possibly reach. You may not be able to work a 40-hour week, for example, but you may be able to work at least part time. In fact, many people find that continuing to work can be helpful.
- Take time for yourself. Eating well, relaxing and getting enough rest can help combat the stress and fatigue of cancer. Also, plan for the downtimes when you may need to rest more or limit what you do.
- Stay active. Receiving a diagnosis of cancer doesn't mean you have to stop doing the things you enjoy or normally do. For the most part, if you feel well enough to do something, go ahead and do it. It's important to stay active and involved as much as you can.
Preparing for your appointment
Make an appointment with your family doctor if you have any signs or symptoms that worry you. If your doctor suspects you have a type of lymphoma, he or she may refer you to a doctor who specializes in diseases that affect blood cells (hematologist).
Because appointments can be brief, and because there's often a lot of information to discuss, it's a good idea to be well prepared. Here's some information to help you get ready, and what to expect from your doctor.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet before testing.
- Write down any symptoms you're experiencing, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medications, vitamins or supplements you're taking.
- Consider taking a family member or friend along. Sometimes it can be difficult to absorb all the information provided during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Write down questions to ask your doctor.
Your time with your doctor is limited, so preparing a list of questions can help you make the most of your time together. List your questions from most important to least important in case time runs out. For non-Hodgkin's lymphoma, some basic questions to ask your doctor include:
- Do I have non-Hodgkin's lymphoma?
- What type of non-Hodgkin's lymphoma do I have?
- How advanced is my cancer?
- Is my condition aggressive or slow growing?
- Will I need more tests?
- Will I need treatment?
- What are my treatment options?
- What are the potential side effects of each treatment?
- How will treatment affect my daily life? Can I continue working?
- How long will treatment last?
- Is there one treatment you feel is best for me?
- If you had a friend or loved one in my situation, what advice would you give that person?
- Should I see a specialist? What will that cost, and will my insurance cover it?
- Do you have brochures or other printed material that I can take with me? What websites do you recommend?
In addition to the questions that you've prepared to ask your doctor, don't hesitate to ask additional questions.
What to expect from your doctor
Your doctor is likely to ask you a number of questions. Being ready to answer them may reserve time to go over points you want to spend more time on. Your doctor may ask:
- When did you first begin experiencing symptoms?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- Have you had infections in the past?
- Have you or your family been exposed to toxins?
Follow us on Twitter
@MayoCancerCare
Oct. 26, 2022