Diagnosis
Hysterosonography
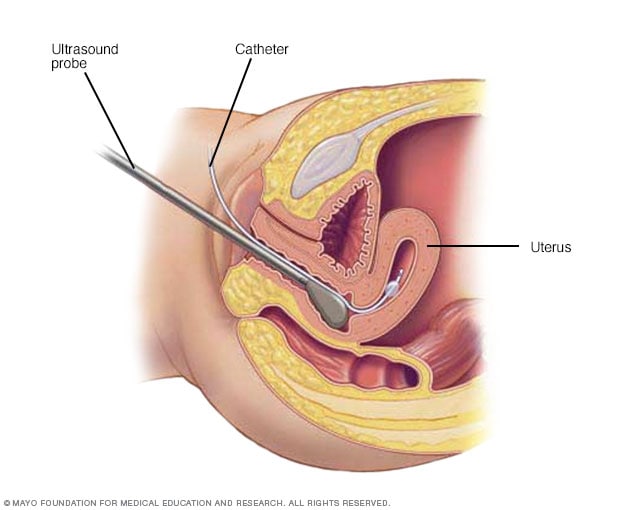
Hysterosonography
During hysterosonography (his-tur-o-suh-NOG-ruh-fee), you have a thin, flexible tube called a catheter placed in the uterus. Salt water, also called saline, is injected through the flexible tube into the hollow part of the uterus. An ultrasound probe transmits images of the inside of the uterus to a nearby monitor.
Hysteroscopy

Hysteroscopy
During hysteroscopy (his-tur-OS-kuh-pee), a thin, lighted instrument provides a view of the inside of the uterus. This instrument also is called a hysteroscope.
A member of your health care team will likely ask about your medical history and menstrual cycles. You may be asked to keep a diary to track days with and without bleeding. Record information such as how heavy your flow was and how many sanitary pads or tampons you needed to control it.
After doing a physical exam, your doctor or other member of your care team may recommend certain tests or procedures. They may include:
- Blood tests. A sample of your blood may be tested for iron deficiency anemia. The sample also may be tested for other conditions, such as thyroid disorders or blood-clotting problems.
- Pap test. In this test, cells from your cervix are collected. They are tested for inflammation or changes that may be precancerous, which means they could lead to cancer. Cells also are tested for human papilloma virus in women ages 25 to 30 and older.
- Endometrial biopsy. Your doctor may take a tissue sample from the inside of your uterus. A pathologist will look for signs of cancer or precancer of the uterus.
- Ultrasound. This imaging method uses sound waves to create pictures of your uterus, ovaries and pelvis.
Results of these initial tests may lead to more testing, including:
- Sonohysterography. During this test, a fluid is injected through a tube into your uterus by way of your vagina and cervix. Your doctor then uses ultrasound to look for problems in the lining of your uterus.
- Hysteroscopy. A thin, lighted instrument is inserted through your vagina and cervix into your uterus. This allows your doctor to see the inside of your uterus.
Your doctor can make a diagnosis of heavy menstrual bleeding or abnormal uterine bleeding only after it's known that something else isn't causing your condition. These causes may include menstrual disorders, medical conditions or medicines.
Treatment
Treatment for heavy menstrual bleeding is based on a number of factors. These include:
- Your overall health and medical history.
- The cause of the condition and how serious it is.
- How well you tolerate certain medicines or procedures.
- The chance that your periods will soon become less heavy.
- Your plans to have children.
- How the condition affects your lifestyle.
- Your opinion or personal choices.
Medicines
Medicines for heavy menstrual bleeding may include:
- Nonsteroidal anti-inflammatory drugs, also called NSAIDs. NSAIDs, such as ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve), help reduce menstrual blood loss. NSAIDs may also make menstrual cramps less painful.
- Tranexamic acid. Tranexamic acid (Lysteda) helps reduce menstrual blood loss. This medicine only needs to be taken at the time of bleeding.
- Oral contraceptives. Aside from birth control, oral contraceptives can help regulate menstrual cycles and ease menstrual bleeding that is heavy or lasts a long time.
- Oral progesterone. The natural hormone progesterone can help fix hormone imbalance and reduce heavy menstrual bleeding. The synthetic form of progesterone is called progestin.
- Hormonal IUD (Mirena, Liletta, others). This intrauterine device releases a type of progestin called levonorgestrel. It makes the uterine lining thin and reduces menstrual blood flow and cramping.
- Other medicines. Gonadotropin-releasing hormone agonists and antagonists are also called GnRH medicines. They help control heavy uterine bleeding. Relugolix combined with an estrogen and progestin (Myfembree) may help control bleeding caused by fibroids. Elagolix with an estrogen and progestin (Oriahnn) is used to treat fibroid-related bleeding. Elagolix alone (Orilissa) may help control bleeding caused by endometriosis.
If you have heavy menstrual bleeding from taking hormone medicine, you may need to stop or change your medicine.
If you have anemia due to heavy menstrual bleeding, you may need to take iron supplements. If your iron levels are low but you're not yet anemic, you may be started on iron supplements instead of waiting until you become anemic.
Procedures
You may need surgery for heavy menstrual bleeding if medicines do not help. Treatment options include:
- Dilation and curettage, also called a D&C. In this procedure, your doctor opens your cervix. This also is called dilating the cervix. The doctor then scrapes or suctions tissue from the lining of your uterus. This also is known as curettage. You may have a D&C to find the source of abnormal uterine bleeding. Causes of bleeding may include polyps, fibroids or cancer of the uterus. If you've had a miscarriage, you may need a D&C to completely empty the uterus. Hysteroscopy is often used with D&C to help doctors find the source of bleeding in the uterus.
- Uterine artery embolization. The goal of this procedure is to block blood flow to uterine fibroids. Blocking blood flow to fibroids helps to shrink them. During the procedure, the surgeon passes a catheter through the large artery in the thigh. This also is known as the femoral artery. The surgeon guides the catheter to the blood vessels in the uterus and injects tiny beads or sponges to reduce blood flow to the fibroid.
- Focused ultrasound. This procedure shrinks fibroids by targeting and destroying fibroids through ultrasound waves and radiofrequency energy. It needs no incisions.
- Myomectomy. This is the surgical removal of uterine fibroids. Depending on the size, number and location of the fibroids, your surgeon may perform the myomectomy through several small incisions in the abdomen. This is known also as the laparoscopic approach. Or the surgeon may put a thin, flexible tube into the vagina and cervix to see and remove fibroids or polyps inside the uterus. This also is called the hysteroscopic approach.
-
Endometrial ablation. This procedure involves destroying the lining of the uterus. The process of destroying tissue also is known as ablation. The surgeon uses a laser, radio waves or heat applied to the lining of the uterus to destroy the tissue.
After endometrial ablation, you may have much lighter periods. Pregnancy after endometrial ablation isn't likely but is possible and could be dangerous. Using reliable or permanent birth control until menopause is recommended.
- Endometrial resection. The surgeon uses an electrosurgical wire loop to remove the lining of the uterus. Pregnancy isn't recommended after this procedure.
- Hysterectomy. In this procedure, the uterus and cervix are removed. It ends menstrual periods and the ability to get pregnant. Hysterectomy is performed under anesthesia and may require a short hospital stay. Early menopause may occur if the ovaries are removed. The procedure to remove both ovaries is called bilateral oophorectomy.
Many of these surgical procedures are done on an outpatient basis. You may need a general anesthetic but it's likely that you can go home on the same day. With an abdominal myomectomy or a hysterectomy, you may need a brief hospital stay.
Sometimes heavy menstrual bleeding is a sign of another condition, such as thyroid disease. In those cases, treating the condition usually results in lighter periods.
More Information
Preparing for your appointment
You may start by seeing your primary care doctor or other health care professional. Or you may be referred immediately to a specialist called an obstetrician/gynecologist.
Here's some information to help you get ready for your appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as fasting before having a specific test. Make a list of:
- Your symptoms, including any that seem unrelated to the reason for your appointment.
- Key personal information, including major stresses, recent life changes and family medical history.
- All medications, vitamins or supplements you take, including the doses.
- Questions to ask your doctor.
Take a family member or friend along, if possible, to help you remember the information you're given.
For heavy menstrual bleeding, some basic questions to ask your care team include:
- What's likely causing my symptoms?
- Other than the most likely cause, what are other possible causes for my symptoms?
- What tests do I need?
- Is my condition likely temporary or will it be ongoing?
- What are my treatment options?
- I have these other health conditions. How can I best manage them together?
- Should I see a specialist?
- Are there brochures or other printed material I can have? What websites do you recommend?
Don't hesitate to ask any other questions as they occur to you during your appointment.
What to expect from your doctor
You may be asked certain questions during your appointment, such as:
- When did your symptoms begin?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, seems to worsen your symptoms?
What you can do in the meantime
Avoid doing anything that seems to worsen your symptoms.
Aug. 30, 2023