Overview
Colon and small intestine
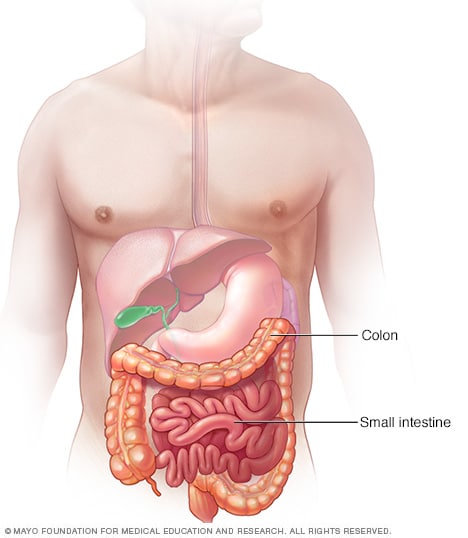
Colon and small intestine
The small intestine and colon are parts of the digestive tract, which processes the foods you eat. The intestines take nutrients from the foods. What isn't absorbed by the intestines moves along the digestive tract and is passed out of the body as stool.
Intestinal ischemia (is-KEE-me-uh) refers to a range of conditions that happen when blood flow to the intestines slows or stops. Ischemia can be due to a fully or partly blocked blood vessel, most often an artery. Or low blood pressure may lead to less blood flow. Intestinal ischemia can affect the small intestine, the large intestine or both.
Less blood flow means that too little oxygen goes to the cells in the system through which food travels, called the digestive system. Intestinal ischemia is a serious condition that can cause pain. It can make it hard for the intestines to work well.
In severe cases, loss of blood flow to the intestines can cause lifelong damage to the intestines. And it may lead to death.
There are treatments for intestinal ischemia. Getting medical help early improves the chances of recovery.
Symptoms
Symptoms of intestinal ischemia can come on quickly. When this happens, the condition is called acute intestinal ischemia. When symptoms come on slowly, the condition is called chronic intestinal ischemia. Symptoms may differ from person to person. But certain symptoms suggest a diagnosis of intestinal ischemia.
Symptoms of sudden intestinal ischemia, also called acute intestinal ischemia
Symptoms of acute intestinal ischemia most often include:
- Sudden belly pain.
- An urgent need to pass stool.
- Forcefully passing stool often.
- Belly tenderness or bloating, also called distention.
- Bloody stools.
- Nausea and vomiting.
- Mental confusion, in older adults.
Symptoms of intestinal ischemia that comes on slowly, also called chronic intestinal ischemia
Symptoms of chronic intestinal ischemia can include:
- Belly cramps or fullness, most often within 30 minutes after eating, that lasts 1 to 3 hours.
- Belly pain that gets worse little by little over weeks or months.
- Fear of eating because of pain after eating.
- Weight loss without trying.
- Diarrhea.
- Nausea and vomiting.
- Bloating.
When to see a doctor
Seek medical care right away if you have sudden, severe belly pain. Pain that feels so bad that you can't sit still or find a position that feels OK is a medical emergency.
If you have other symptoms that worry you, make an appointment with your healthcare professional.
Causes
Intestinal ischemia happens when the blood flow through the major blood vessels that send blood to and from the intestines slows or stops. The condition has many possible causes. Causes may include:
- A blood clot that blocks an artery.
- A narrowed artery due to buildup of fatty deposits, such as cholesterol. This condition is called atherosclerosis.
- Low blood pressure leading to less blood flow.
- Blockage in a vein, which happens less often.
Intestinal ischemia often is split into groups. Colon ischemia, also called ischemic colitis, affects the large intestine. Other types of ischemia affect the small intestine. These are acute mesenteric ischemia, chronic mesenteric ischemia and ischemia due to mesenteric venous thrombosis.
Colon ischemia, also called ischemic colitis
This type of intestinal ischemia is the most common. It happens when blood flow to part of the colon slows or gets blocked. The cause of less blood flow to the colon isn't always clear. But conditions that can raise the risk of colon ischemia include:
- Very low blood pressure, called hypotension. This may be linked to heart failure, major surgery, trauma, shock or loss of body fluids, called dehydration.
- A blood clot or severe block in an artery that sends blood to the colon. This is called atherosclerosis.
- A twist of the bowel, called volvulus, or the trapping of intestinal contents within a hernia.
- An enlarged bowel from scar tissue or a tumor blocking the bowel.
- Other medical conditions that affect the blood. These include lupus, sickle cell anemia, and swelling and irritation, called inflammation, of the blood vessels. This inflammation is known as vasculitis.
- Medicines that narrow blood vessels. These include some that treat heart disease and migraine.
- Hormonal medicines, such as birth control pills.
- Cocaine or methamphetamine use.
- Intense exercise, such as long-distance running.
Acute mesenteric ischemia
Mesenteric ischemia happens when narrowed or blocked arteries restrict blood flow to the small intestine. This can cause lifelong damage to the small intestine.
Acute mesenteric ischemia is the result of a sudden loss of blood flow to the small intestine. It may be due to:
-
A blood clot, also called an embolus, that comes loose in the heart and travels through the blood to block an artery. It most often blocks the superior mesenteric artery, which sends oxygen-rich blood to the intestines.
This is the most common cause of acute mesenteric artery ischemia. Congestive heart failure, a heart attack or an irregular heartbeat, called an arrhythmia, can bring it on.
- A blockage that happens in one of the main intestinal arteries. This often is a result of atherosclerosis. This type of sudden ischemia tends to happen in people with chronic intestinal ischemia.
-
Slowed blood flow from low blood pressure. Low blood pressure may be due to shock, heart failure, certain medicines or ongoing kidney failure, called chronic kidney failure. Slowed blood flow is more common in people who have other serious illnesses and fatty deposits on an artery wall, called atherosclerosis.
This type of acute mesenteric ischemia often is called nonocclusive ischemia. This means it's not due to a blockage in the artery.
Chronic mesenteric ischemia
Chronic mesenteric ischemia is due to the buildup of fatty deposits on an artery wall, called atherosclerosis. The disease process most often is slow. It's also called intestinal angina because it's due to less blood flow to the intestines after eating.
You may not need treatment until at least two of the three major arteries that send blood to your intestines become very narrow or blocked all the way.
A possible dangerous complication of chronic mesenteric ischemia is having a blood clot within a narrowed artery. This can cause a sudden blockage, which can cause acute mesenteric ischemia.
Ischemia due to mesenteric venous thrombosis
This type of ischemia happens when blood can't leave the small intestine. This can be due to a blood clot in a vein that drains blood from the intestines. Veins carry blood back to the heart after the oxygen is removed. When the vein is blocked, blood backs up in the intestines, causing swelling and bleeding.
This may result from:
- Acute or chronic irritation and swelling, called inflammation, of the pancreas. This condition is called pancreatitis.
- Infection inside the belly.
- Cancers of the digestive system.
- Bowel diseases, such as ulcerative colitis, Crohn's disease or diverticulitis.
- Conditions that make the blood clot more easily.
- Medicines such as estrogen that can raise clotting risk.
- Injuries to the belly area.
Risk factors
Factors that may increase your risk of intestinal ischemia include:
- Buildup of fatty deposits in your arteries, called atherosclerosis. If you've had other conditions caused by atherosclerosis, you have an increased risk of intestinal ischemia. These conditions include less blood flow to the heart, called coronary artery disease; less blood flow to the legs, called peripheral vascular disease; or less blood flow to the arteries that go to the brain, called carotid artery disease.
- Age. People older than 50 are more likely to get intestinal ischemia.
- Smoking. Using cigarettes and other forms of smoked tobacco increases your risk of intestinal ischemia.
- Heart and blood vessel conditions. Your risk of intestinal ischemia is higher if you have congestive heart failure or an irregular heartbeat such as atrial fibrillation. Blood vessel diseases that result in irritation, called inflammation, of veins and arteries also may increase risk. This inflammation is known as vasculitis.
- Medicines. Certain medicines may increase your risk of intestinal ischemia. Examples include birth control pills and medicines that cause your blood vessels to expand or contract, such as some allergy medicines and migraine medicines.
- Blood-clotting problems. Diseases and conditions that raise your risk of blood clots also may raise your risk of intestinal ischemia. Examples include sickle cell anemia and a genetic condition known as the factor V Leiden mutation.
- Other health conditions. Having high blood pressure, diabetes or high cholesterol can increase the risk of intestinal ischemia.
- Illicit drug use. Cocaine and methamphetamine use have been linked to intestinal ischemia.
Complications
Complications of intestinal ischemia can include:
- Death of intestinal tissue. A sudden and complete blockage in blood flow to the intestines can kill intestinal tissue. This is called gangrene.
- A hole through the wall of the intestines, called a perforation. A hole can cause what's in the intestine to leak into the belly. This may cause a serious infection called peritonitis.
- Scarring or narrowing of the intestine. Sometimes the intestines recover from ischemia. But as part of the healing process, the body forms scar tissue that narrows or blocks the intestines. This happens most often in the colon. Rarely, this happens in the small intestine.
Other health conditions, such as chronic obstructive pulmonary disease, also called COPD, can make intestinal ischemia worse. Emphysema, a type of COPD, and other smoking-related lung diseases increase this risk.
Sometimes, intestinal ischemia can be fatal.
Sept. 11, 2024