Diagnosis
Endometriosis FAQs
Get answers to the most frequently asked questions about endometriosis from Megan Wasson, D.O., a minimally invasive gynecologic surgeon at Mayo Clinic.
Hi, I'm Dr. Megan Wasson, a minimally invasive gynecologic surgeon at Mayo Clinic. I'm here to answer some of the important questions that you might have about endometriosis.
What causes endometriosis?
I wish I could tell you the answer to that, but unfortunately, we don't know. Currently, we think that the likely source of endometriosis is actually occurring during development as a fetus. So when a baby is developing inside the uterus of its mother, that's when we think endometriosis actually starts.
How do I know if I have endometriosis?
That's a really great question. So endometriosis is something that can be a little bit elusive, but we can suspect it based on symptoms that you might be experiencing. If you're having pain with your periods, pain in your pelvis in general pain with intercourse, urination, bowel movements, all of that may point us to a suspicion of endometriosis. But unfortunately, the only way to say 100% If you do or do not have endometriosis is to do surgery. Because during surgery we can remove tissue, look at it underneath the microscope, and definitively be able to say whether you do or do not have endometriosis.
Can endometriosis be seen on imaging?
Unfortunately, most of the time, no. The vast majority of endometriosis is superficial endometriosis, meaning that it's almost like paint spackling on a wall, that we can't see it unless we actually go in and take a look surgically. The exception to that is if there's endometriosis actually growing into organs in the pelvis or the abdomen like the bowel or the bladder. That's called deep-infiltrating endometriosis. In those scenarios, we can frequently see that disease either on ultrasound or on MRI.
If I have endometriosis, should I have a hysterectomy?
Not necessarily. So endometriosis, it's cells similar to the lining of the uterus that are growing outside of the uterus. So it's truly not an issue with the uterus at all, which is what we treat with hysterectomy. That being said, there is a sister condition to endometriosis called adenomyosis and that occurs concurrently in 80 to 90% of patients, and so with adenomyosis, the uterus itself can be a source of problems, including pain. In those scenarios, sometimes we do consider a hysterectomy at the time that we're treating endometriosis.
What happens if my endometriosis is left untreated?
The key thing to remember here is that endometriosis is a progressive condition, and it will continue to grow and may cause progressive symptoms. So for some patients, that means that initially the pain was only with the menstrual cycle. But over time with that progression of disease, the pain can start to occur outside of the cycle, so throughout different times of the month, with urination, with bowel movements, with intercourse. So that can prompt us to need to intervene and do treatment if we hadn't done anything previously. But that being said, even though we know endometriosis is progressive, for some patients, it doesn't ever progress to the point that we would need to do any treatment because it's more of a quality of life issue. And if it's not impacting the quality of life, we don't really need to do anything.
Can I become pregnant if I have endometriosis?
100%. You can absolutely have children if you have endometriosis. When we talk about infertility, those are patients who are struggling with pregnancy already. But if we look at all patients with endometriosis, everyone with that diagnosis, the vast majority are able to achieve pregnancy without any problem whatsoever. They can get pregnant, they can carry the pregnancy. They walk home from the hospital with a beautiful baby in their arms. So, yes, unfortunately, infertility can be associated with endometriosis. But the vast majority of the time, it's truly not a problem.
How can I be the best partner to my medical team?
Being a partner for the medical team is truly key. A lot of individuals with endometriosis have been in pain for a prolonged period of time, which unfortunately means that the body has changed in response. And pain has almost become like an onion with endometriosis at the core of that onion. So we need to work not only to treat the endometriosis, but treat other potential sources of pain that have arisen. And so I encourage you to educate yourself, not only so that you can come in to your health care provider and have a dialogue and a conversation as to what you need and what you're experiencing. But also so you can be an advocate and make sure that you are getting the health care that you need and that you deserve. Also talk about it. Know women have, for years and decades, been told that a period is supposed to be painful and we just have to unfortunately suck it up and deal with it. That's not the reality. The reality is we should not be laying on the bathroom floor when we have our period. We should not be crying during intercourse. That is not normal. If you're experiencing it, speak up. Talk to your family, Talk to your friends. Talk to your health care provider. Let them know what's going on. Because truly, we are here to help and together we can start to make a impact not only on endometriosis for you, but endometriosis in society as a whole. Never hesitate to ask your medical team any questions or concerns you have. Being informed truly makes all the difference. Thanks for your time and we wish you well.
Pelvic exam
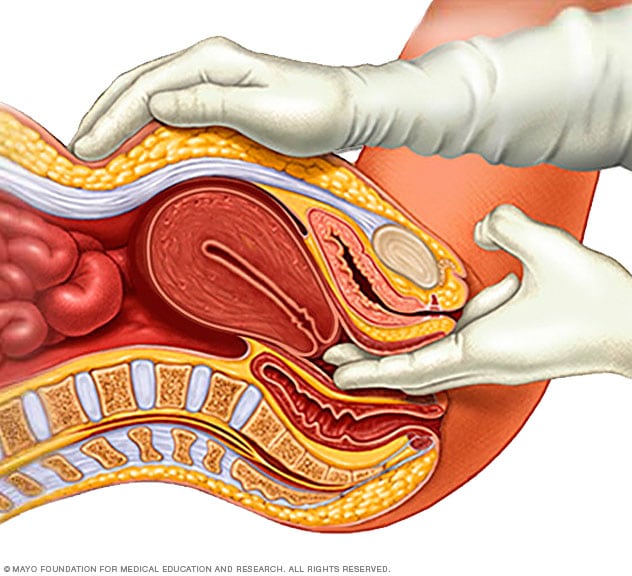
Pelvic exam
During a pelvic exam, a doctor inserts one or two gloved fingers inside the vagina. Pressing down on the abdomen at the same time, the doctor can check the uterus, ovaries and other organs.
Transvaginal ultrasound
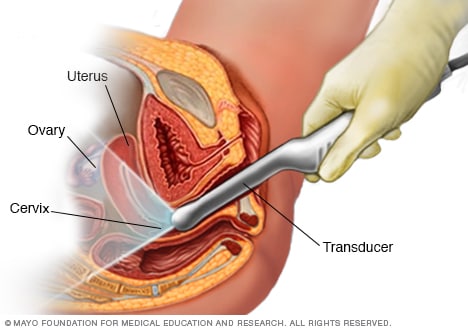
Transvaginal ultrasound
During a transvaginal ultrasound, a healthcare professional or technician uses a wandlike device called a transducer. The transducer is inserted into your vagina while you lie on your back on an exam table. The transducer emits sound waves that generate images of your pelvic organs.
To find out if you have endometriosis, your doctor will likely start by giving you a physical exam. You'll be asked to describe your symptoms, including where and when you feel pain.
Tests to check for clues of endometriosis include:
- Pelvic exam. Your health care professional feels areas in your pelvis with one or two gloved fingers to check for any unusual changes. These changes can include cysts on the reproductive organs, painful spots, irregular growths called nodules and scars behind the uterus. Often, small areas of endometriosis can't be felt unless a cyst has formed.
- Ultrasound. This test uses sound waves to make pictures of the inside of the body. To capture the images, a device called a transducer might be pressed against the stomach area. Or it may be placed into the vagina in a version of the exam called transvaginal ultrasound. Both types of the test may be done to get the best view of the reproductive organs. A standard ultrasound won't confirm whether you have endometriosis. But it can find cysts linked with the condition called endometriomas.
- Magnetic resonance imaging (MRI). This exam uses a magnetic field and radio waves to make images of the organs and tissues within the body. For some, an MRI helps with surgical planning. It gives your surgeon detailed information about the location and size of endometriosis growths.
-
Laparoscopy. In some cases, you may be referred to a surgeon for this procedure. Laparoscopy lets the surgeon check inside your abdomen for signs of endometriosis tissue. Before the surgery, you receive medicine that puts you a sleep-like state and prevents pain. Then your surgeon makes a tiny cut near your navel and inserts a slender viewing instrument called a laparoscope.
A laparoscopy can provide information about the location, extent and size of the endometriosis growths. Your surgeon may take a tissue sample called biopsy for more testing. With proper planning, a surgeon can often treat endometriosis during the laparoscopy so that you need only one surgery.
Treatment
Treatment for endometriosis often involves medicine or surgery. The approach you and your health care team choose will depend on how serious your symptoms are and whether you hope to become pregnant.
Typically, medicine is recommended first. If it doesn't help enough, surgery becomes an option.
Pain medicines
Your health care team may recommend pain relievers that you can buy without a prescription. These medicines include the nonsteroidal anti-inflammatory drugs (NSAIDs) ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve). They can help ease painful menstrual cramps.
Your care team may recommend hormone therapy along with pain relievers if you're not trying to get pregnant.
Hormone therapy
Sometimes, hormone medicine help ease or get rid of endometriosis pain. The rise and fall of hormones during the menstrual cycle causes endometriosis tissue to thicken, break down and bleed. Lab-made versions of hormones may slow the growth of this tissue and prevent new tissue from forming.
Hormone therapy isn't a permanent fix for endometriosis. The symptoms could come back after you stop treatment.
Therapies used to treat endometriosis include:
- Hormonal contraceptives. Birth control pills, shots, patches and vaginal rings help control the hormones that stimulate endometriosis. Many have lighter and shorter menstrual flow when they use hormonal birth control. Using hormonal contraceptives may ease or get rid of pain in some cases. The chances of relief seem to go up if you use birth control pills for a year or more with no breaks.
- Gonadotropin-releasing hormone (Gn-RH) agonists and antagonists. These medicines block the menstrual cycle and lower estrogen levels. This causes endometriosis tissue to shrink. These medicines create an artificial menopause. Taking a low dose of estrogen or progestin along with Gn-RH agonists and antagonists may ease menopausal side effects. Those include hot flashes, vaginal dryness and bone loss. Menstrual periods and the ability to get pregnant return when you stop taking the medicine.
- Progestin therapy. Progestin is a lab-made version of a hormone that plays a role in the menstrual cycle and pregnancy. A variety of progestin treatments can stop menstrual periods and the growth of endometriosis tissue, which may relieve symptoms. Progestin therapies include a tiny device placed in the uterus that releases levonorgestrel (Mirena, Skyla, others), a contraceptive rod placed under the skin of the arm (Nexplanon), birth control shots (Depo-Provera) or a progestin-only birth control pill (Camila, Slynd).
- Aromatase inhibitors. These are a class of medicines that lower the amount of estrogen in the body. Your health care team may recommend an aromatase inhibitor along with a progestin or combination birth control pills to treat endometriosis.
Conservative surgery
Conservative surgery removes endometriosis tissue. It aims to preserve the uterus and the ovaries. If you have endometriosis and you're trying to become pregnant, this type of surgery may boost your chances of success. It also may help if the condition causes you terrible pain — but endometriosis and pain may come back over time after surgery.
Your surgeon may do this procedure with small cuts, also called laparoscopic surgery. Less often, surgery that involves a larger cut in the abdomen is needed to remove thick bands of scar tissue. But even in severe cases of endometriosis, most can be treated with the laparoscopic method.
During laparoscopic surgery, your surgeon places a slender viewing instrument called a laparoscope through a small cut near your navel. Surgical tools are inserted to remove endometriosis tissue through another small cut. Some surgeons do laparoscopy with help from robotic devices that they control. After surgery, your health care team may recommend taking hormone medicine to help improve pain.
Fertility treatment
Endometriosis can lead to trouble getting pregnant. If you have a hard time conceiving, your health care team may recommend fertility treatment. You might be referred to a doctor who treats infertility, called a reproductive endocrinologist. Fertility treatment can include medicine that helps ovaries make more eggs. It also can include a series of procedures that mix eggs and sperm outside the body, called in vitro fertilization. The treatment that's right for you depends on your personal situation.
Hysterectomy with removal of the ovaries
Hysterectomy is surgery to remove the uterus. Taking out the uterus and ovaries was once thought to be the most effective treatment for endometriosis. Today, some experts consider it to be a last resort to ease pain when other treatments haven't worked. Other experts instead recommend surgery that focuses on the careful and thorough removal of all endometriosis tissue.
Having the ovaries removed, also called oophorectomy, causes early menopause. The lack of hormones made by the ovaries may improve endometriosis pain for some. But for others, endometriosis that remains after surgery continues to cause symptoms. Early menopause also carries a risk of heart and blood vessel diseases, certain metabolic conditions and early death.
In people who don't want to get pregnant, hysterectomy sometimes can be used to treat symptoms linked with endometriosis. These include heavy menstrual bleeding and painful menses due to uterine cramping. Even when the ovaries are left in place, a hysterectomy may still have a long-term effect on your health. That's especially true if you have the surgery before age 35.
To manage and treat endometriosis, it's key to find a health care professional with whom you feel comfortable. You may want to get a second opinion before you start any treatment. That way, you can be sure you know all of your options and the pros and cons of each.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
It may take time to find a treatment that works. Until then, you can try some things at home to ease your pain.
- Warm baths and a heating pad can help relax pelvic muscles. This lessens cramping and pain.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) can help ease painful menstrual cramps. NSAIDs include ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve).
You also can ask your health care team if physical therapy might help. A therapist can teach you how to relax muscles that support the uterus, called the pelvic floor. Relaxing these tight muscles may help pelvic pain linked with endometriosis feel less intense.
Alternative medicine
Alternative medicine involves treatments that aren't part of standard medical care. Some people with endometriosis say they get pain relief from alternative therapies such as:
- Acupuncture, in which a trained practitioner places fine needles into the skin.
- Chiropractic care, in which a licensed professional adjusts the spine or other body parts.
- Herbs such as cinnamon trig or licorice root.
- Supplements including vitamin B1, magnesium or omega-3 fatty acids.
Acupuncture has shown some promise at easing endometriosis pain. But overall, there's little research on much relief people with the condition might get from alternative medicine. Always check with your health care team before you try a new alternative therapy to find out if it's safe for you. For example, supplements and herbs can affect standard treatments such as medicines. If you're interested in trying acupuncture or chiropractic care, ask your care team to recommend reputable professionals. Check with your insurance company to see if the expense will be covered.
Coping and support
Think about joining a support group if you have endometriosis or a complication such as fertility trouble. Sometimes it helps simply to talk to other people who can relate to your feelings and experiences. If you can't find a support group in your community, look for one online.
Preparing for your appointment
Your first appointment will likely be with either your primary care doctor or a gynecologist. If you're seeking treatment for infertility, you may be referred to a doctor called a reproductive endocrinologist.
Appointments can be brief, and it can be hard to remember everything you want to discuss. So it's a good idea to plan ahead for your appointment.
What you can do
- Make a list of any symptoms you have. Include all of your symptoms, even if you don't think they're related to the reason for your appointment.
- Make a list of any medicines, herbs or vitamin supplements you take. Include how often you take them and how much you take, called the dose.
- Have a family member or close friend join you, if possible. You may get a lot of information at your visit, and it can be hard to recall everything.
- Take a notepad or electronic device with you. Use it to make notes of important information during your visit.
- Prepare a list of questions to ask your doctor. List your most important questions first, to be sure you bring up those points.
For endometriosis, some basic questions to ask your doctor include:
- How is endometriosis diagnosed?
- What medicines treat endometriosis? Is there a medicine that can ease my symptoms?
- What side effects can I expect from medicine?
- Do you recommend surgery?
- Will endometriosis affect my ability to become pregnant?
- Can treatment of endometriosis improve my fertility?
- Can you recommend any alternative treatments I might try?
Make sure that you understand everything your health care team tells you. It's fine to ask your team to repeat information or to ask follow-up questions.
What to expect from your doctor
Some questions your doctor might ask include:
- How often do you have these symptoms?
- How long have you had these symptoms?
- How bad are your symptoms?
- Do your symptoms seem to be related to your menstrual cycle?
- Does anything improve your symptoms?
- Does anything make your symptoms worse?
Aug. 30, 2024