Overview
Diabetes insipidus (die-uh-BEE-teze in-SIP-uh-dus) is an uncommon problem that causes the fluids in the body to become out of balance. That prompts the body to make large amounts of urine. It also causes a feeling of being very thirsty even after having something to drink. Diabetes insipidus also is called arginine vasopressin deficiency and arginine vasopressin resistance.
While the terms "diabetes insipidus" and "diabetes mellitus" sound alike, the two conditions are not connected. Diabetes mellitus involves high blood sugar levels. It's a common condition, and it's often called simply diabetes.
There's no cure for diabetes insipidus. But treatment is available that can ease its symptoms. That includes relieving thirst, lowering the amount of urine the body makes and preventing dehydration.
Products & Services
Symptoms
Symptoms of diabetes insipidus in adults include:
- Being very thirsty, often with a preference for cold water.
- Making large amounts of pale urine.
- Getting up to urinate and drink water often during the night.
Adults typically urinate an average of 1 to 3 quarts (about 1 to 3 liters) a day. People who have diabetes insipidus and who drink a lot of fluids may make as much as 20 quarts (about 19 liters) of urine a day.
A baby or young child who has diabetes insipidus may have these symptoms:
- Large amounts of pale urine that result in heavy, wet diapers.
- Bed-wetting.
- Being very thirsty, with a preference for drinking water and cold liquids.
- Weight loss.
- Poor growth.
- Vomiting.
- Irritability.
- Fever.
- Constipation.
- Headache.
- Problems sleeping.
- Vision problems.
When to see a doctor
See your health care provider right away if you notice that you're urinating much more than usual and you're very thirsty on a regular basis.
Causes
Female urinary system
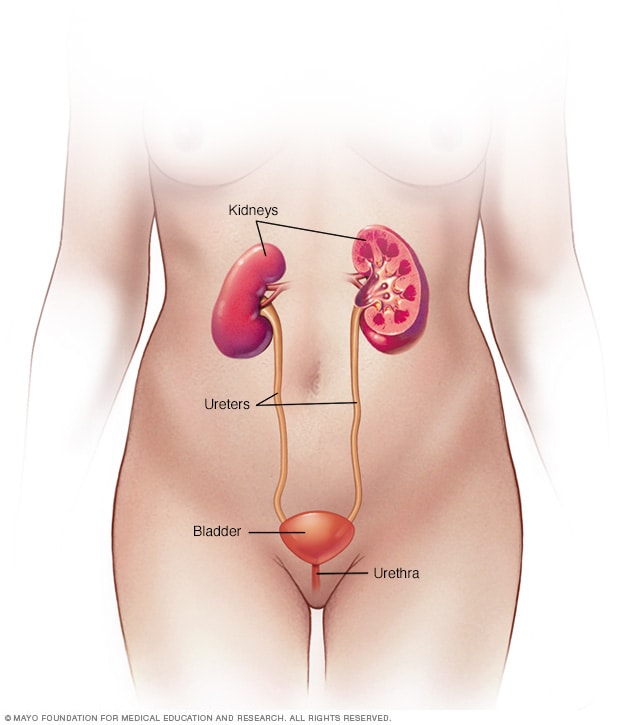
Female urinary system
The urinary system includes the kidneys, ureters, bladder and urethra. The urinary system removes waste from the body through urine. The kidneys sit toward the back of the upper abdomen. They filter waste and fluid from the blood and make urine. Urine moves from the kidneys to the bladder through narrow tubes called the ureters. The bladder stores urine until it's time to urinate. Urine leaves the body through a small tube called the urethra.
Pituitary gland and hypothalamus
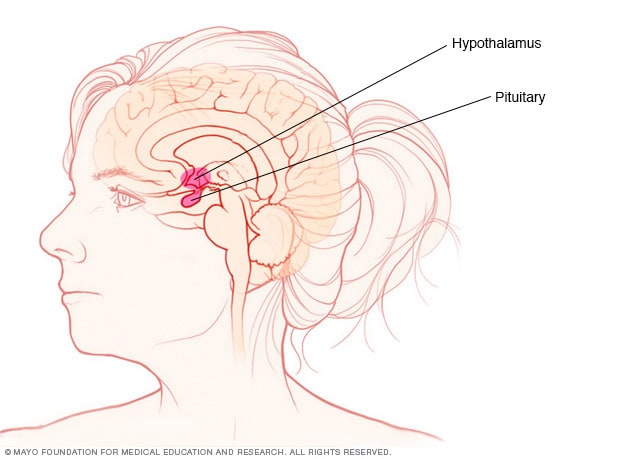
Pituitary gland and hypothalamus
The pituitary gland and the hypothalamus are located within the brain and control hormone production.
Diabetes insipidus happens when the body can't balance its fluid levels in a healthy way.
Fluid in the blood is filtered through the kidneys to remove waste. Afterward, most of that fluid is returned to the bloodstream. The waste and a small amount of fluid leave the kidneys as urine. Urine leaves the body after it's temporarily stored in the bladder.
A hormone known as antidiuretic hormone (ADH) — also called vasopressin — is needed to get the fluid that's filtered by the kidneys back into the bloodstream. ADH is made in a part of the brain called the hypothalamus. It's then stored in the pituitary gland, a small gland found at the base of the brain. Conditions that cause the brain to make too little ADH or disorders that block the effect of ADH cause the body to make too much urine.
In diabetes insipidus, the body can't properly balance fluid levels. The cause of the fluid imbalance depends on the type of diabetes insipidus.
- Central diabetes insipidus. Damage to the pituitary gland or hypothalamus from surgery, a tumor, a head injury or an illness can cause central diabetes insipidus. That damage affects the production, storage and release of ADH. An inherited disorder may cause this condition too. It also can be the result of an autoimmune reaction that causes the body's immune system to damage the cells that make ADH.
- Nephrogenic diabetes insipidus. This happens when there's a problem with the kidneys that makes them unable to properly respond to ADH. That problem may be due to:
- An inherited disorder.
- Certain medicines, including lithium and antiviral medicines such as foscarnet (Foscavir).
- Low levels of potassium in the blood.
- High levels of calcium in the blood.
- A blocked urinary tract or a urinary tract infection.
- A chronic kidney condition.
- Gestational diabetes insipidus. This rare form of diabetes insipidus only happens during pregnancy. It develops when an enzyme made by the placenta destroys ADH in a pregnant person.
- Primary polydipsia. This condition also is called dipsogenic diabetes insipidus. People who have this disorder constantly feel thirsty and drink lots of fluids. It can be caused by damage to the thirst-regulating mechanism in the hypothalamus. It also has been linked to mental illness, such as schizophrenia.
Sometimes no clear cause of diabetes insipidus can be found. In that case, repeat testing over time often is useful. Testing may be able to identify an underlying cause eventually.
Risk factors
Anyone can get diabetes insipidus. But those at higher risk include people who:
- Have a family history of the disorder.
- Take certain medicines, such as diuretics, that could lead to kidney problems.
- Have high levels of calcium or low levels of potassium in their blood.
- Have had a serious head injury or brain surgery.
Complications
Dehydration
Diabetes insipidus may lead to dehydration. That happens when the body loses too much fluid. Dehydration can cause:
- Dry mouth.
- Thirst.
- Extreme tiredness.
- Dizziness.
- Lightheadedness.
- Fainting.
- Nausea.
Electrolyte imbalance
Diabetes insipidus can change the levels of minerals in the blood that maintain the body's balance of fluids. Those minerals, called electrolytes, include sodium and potassium. Symptoms of an electrolyte imbalance may include:
- Weakness.
- Nausea.
- Vomiting.
- Loss of appetite.
- Confusion.