Overview
Conjoined twins
Conjoined twins
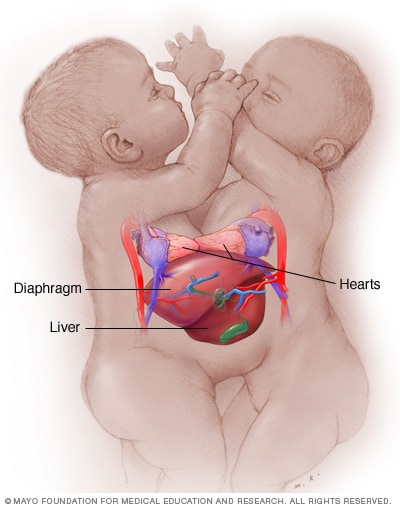
Conjoined twins may be joined at one of several places. These conjoined twins are joined at the chest (thoracopagus). They have separate hearts but share other organs.
Conjoined twins are two babies who are born physically connected to each other.
Conjoined twins develop when an early embryo only partially separates to form two individuals. Although two babies develop from this embryo, they remain physically connected — most often at the chest, abdomen or pelvis. Conjoined twins may also share one or more internal body organs.
Though many conjoined twins are not alive when born (stillborn) or die shortly after birth, advances in surgery and technology have improved survival rates. Some surviving conjoined twins can be surgically separated. The success of surgery depends on where the twins are joined and how many and which organs are shared. It also depends on the experience and skill of the surgical team.
Products & Services
Symptoms
There are no specific symptoms that indicate a conjoined twin pregnancy. As with other twin pregnancies, the uterus may grow faster than it does with a single baby. And there may be more tiredness, nausea and vomiting early in the pregnancy. Conjoined twins can be diagnosed early in the pregnancy using an ultrasound.
How twins are joined
Conjoined twins are usually classified according to where they're joined. The twins sometimes share organs or other parts of their bodies. Each pair of conjoined twins is unique.
Conjoined twins may be joined at any of these sites:
- Chest. Thoracopagus (thor-uh-KOP-uh-gus) twins are joined face to face at the chest. They often have a shared heart and may also share one liver and upper intestine. This is one of the most common sites of conjoined twins.
- Abdomen. Omphalopagus (om-fuh-LOP-uh-gus) twins are joined near the bellybutton. Many omphalopagus twins share the liver and some part of the upper digestive (gastrointestinal or GI) tract. Some twins share the lower part of the small intestine (ileum) and the longest part of the large intestine (colon). They generally do not share a heart.
- Base of spine. Pygopagus (pie-GOP-uh-gus) twins are commonly joined back to back at the base of the spine and the buttocks. Some pygopagus twins share the lower gastrointestinal (GI) tract. A few twins share the genital and urinary organs.
- Length of spine. Rachipagus (ray-KIP-uh-gus), also called rachiopagus (ray-kee-OP-uh-gus), twins are joined back to back along the length of the spine. This type is very rare.
- Pelvis. Ischiopagus (is-kee-OP-uh-gus) twins are joined at the pelvis, either face to face or end to end. Many ischiopagus twins share the lower GI tract, as well as the liver and genital and urinary tract organs. Each twin may have two legs or, less commonly, the twins share two or three legs.
- Trunk. Parapagus (pa-RAP-uh-gus) twins are joined side to side at the pelvis and part or all of the belly (abdomen) and chest, but with separate heads. The twins can have two, three or four arms and two or three legs.
- Head. Craniopagus (kray-nee-OP-uh-gus) twins are joined at the back, top or side of the head, but not the face. Craniopagus twins share a portion of the skull. But their brains are usually separate, though they may share some brain tissue.
- Head and chest. Cephalopagus (sef-uh-LOP-uh-gus) twins are joined at the head and upper body. The faces are on opposite sides of a single shared head, and they share a brain. These twins rarely survive.
In rare cases, twins may be conjoined with one twin smaller and less fully formed than the other (asymmetric conjoined twins). In extremely rare cases, one twin may be found partially developed within the other twin (fetus in fetu).
Causes
Identical twins (monozygotic twins) occur when a single fertilized egg splits and develops into two individuals. Eight to 12 days after conception, the embryonic layers that split to form monozygotic twins begin to develop into specific organs and structures.
It's believed that when the embryo splits later than this — usually between 13 and 15 days after conception — separation stops before the process is complete. The resulting twins are conjoined.
An alternative theory suggests that two separate embryos may somehow fuse together in early development.
What might cause either chain of events to occur is unknown.
Risk factors
Because conjoined twins are so rare, and the cause isn't clear, it's unknown what might make some couples more likely to have conjoined twins.
Complications
Pregnancy with conjoined twins is complex and greatly increases the risk of serious complications. Conjoined babies require surgical delivery by cesarean section (C-section).
As with twins, conjoined babies are likely to be born prematurely, and one or both could be stillborn or die shortly after birth. Severe health issues for twins can occur immediately, such as trouble breathing or heart problems. Later in life, health issues such as scoliosis, cerebral palsy or learning disabilities may occur.
Possible complications depend on where the twins are joined, which organs or other parts of the body they share, and the expertise and experience of the health care team. When conjoined twins are expected, the family and the health care team need to discuss in detail the possible complications and how to prepare for them.
Dec. 16, 2022