Overview
Asthma attack
Asthma attack
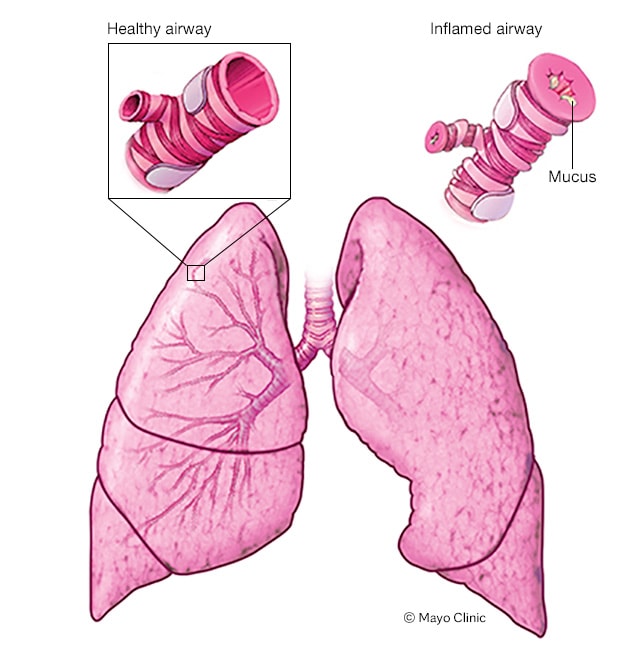
When a person has asthma, the inside walls of the airways in the lungs can narrow and swell. Also, the airway linings may make too much mucus. The result is an asthma attack. During an asthma attack, narrowed airways make breathing difficult and may cause coughing and wheezing.
Asthma is a condition in which your airways narrow and swell and may produce extra mucus. This can make breathing difficult and trigger coughing, a whistling sound (wheezing) when you breathe out and shortness of breath.
For some people, asthma is a minor nuisance. For others, it can be a major problem that interferes with daily activities and may lead to a life-threatening asthma attack.
Asthma can't be cured, but its symptoms can be controlled. Because asthma often changes over time, it's important that you work with your doctor to track your signs and symptoms and adjust your treatment as needed.
Symptoms
Asthma symptoms vary from person to person. You may have infrequent asthma attacks, have symptoms only at certain times — such as when exercising — or have symptoms all the time.
Asthma signs and symptoms include:
- Shortness of breath
- Chest tightness or pain
- Wheezing when exhaling, which is a common sign of asthma in children
- Trouble sleeping caused by shortness of breath, coughing or wheezing
- Coughing or wheezing attacks that are worsened by a respiratory virus, such as a cold or the flu
Signs that your asthma is probably worsening include:
- Asthma signs and symptoms that are more frequent and bothersome
- Increasing difficulty breathing, as measured with a device used to check how well your lungs are working (peak flow meter)
- The need to use a quick-relief inhaler more often
For some people, asthma signs and symptoms flare up in certain situations:
- Exercise-induced asthma, which may be worse when the air is cold and dry
- Occupational asthma, triggered by workplace irritants such as chemical fumes, gases or dust
- Allergy-induced asthma, triggered by airborne substances, such as pollen, mold spores, cockroach waste, or particles of skin and dried saliva shed by pets (pet dander)
When to see a doctor
Seek emergency treatment
Severe asthma attacks can be life-threatening. Work with your doctor to determine what to do when your signs and symptoms worsen — and when you need emergency treatment. Signs of an asthma emergency include:
- Rapid worsening of shortness of breath or wheezing
- No improvement even after using a quick-relief inhaler
- Shortness of breath when you are doing minimal physical activity
Contact your doctor
See your doctor:
- If you think you have asthma. If you have frequent coughing or wheezing that lasts more than a few days or any other signs or symptoms of asthma, see your doctor. Treating asthma early may prevent long-term lung damage and help keep the condition from getting worse over time.
- To monitor your asthma after diagnosis. If you know you have asthma, work with your doctor to keep it under control. Good long-term control helps you feel better from day to day and can prevent a life-threatening asthma attack.
-
If your asthma symptoms get worse. Contact your doctor right away if your medication doesn't seem to ease your symptoms or if you need to use your quick-relief inhaler more often.
Don't take more medication than prescribed without consulting your doctor first. Overusing asthma medication can cause side effects and may make your asthma worse.
- To review your treatment. Asthma often changes over time. Meet with your doctor regularly to discuss your symptoms and make any needed treatment adjustments.
Causes
It isn't clear why some people get asthma and others don't, but it's probably due to a combination of environmental and inherited (genetic) factors.
Asthma triggers
Exposure to various irritants and substances that trigger allergies (allergens) can trigger signs and symptoms of asthma. Asthma triggers are different from person to person and can include:
- Airborne allergens, such as pollen, dust mites, mold spores, pet dander or particles of cockroach waste
- Respiratory infections, such as the common cold
- Physical activity
- Cold air
- Air pollutants and irritants, such as smoke
- Certain medications, including beta blockers, aspirin, and nonsteroidal anti-inflammatory drugs, such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve)
- Strong emotions and stress
- Sulfites and preservatives added to some types of foods and beverages, including shrimp, dried fruit, processed potatoes, beer and wine
- Gastroesophageal reflux disease (GERD), a condition in which stomach acids back up into your throat
Risk factors
A number of factors are thought to increase your chances of developing asthma. They include:
- Having a blood relative with asthma, such as a parent or sibling
- Having another allergic condition, such as atopic dermatitis — which causes red, itchy skin — or hay fever — which causes a runny nose, congestion and itchy eyes
- Being overweight
- Being a smoker
- Exposure to secondhand smoke
- Exposure to exhaust fumes or other types of pollution
- Exposure to occupational triggers, such as chemicals used in farming, hairdressing and manufacturing
Complications
Asthma complications include:
- Signs and symptoms that interfere with sleep, work and other activities
- Sick days from work or school during asthma flare-ups
- A permanent narrowing of the tubes that carry air to and from your lungs (bronchial tubes), which affects how well you can breathe
- Emergency room visits and hospitalizations for severe asthma attacks
- Side effects from long-term use of some medications used to stabilize severe asthma
Proper treatment makes a big difference in preventing both short-term and long-term complications caused by asthma.
Prevention
While there's no way to prevent asthma, you and your doctor can design a step-by-step plan for living with your condition and preventing asthma attacks.
-
Follow your asthma action plan. With your doctor and health care team, write a detailed plan for taking medications and managing an asthma attack. Then be sure to follow your plan.
Asthma is an ongoing condition that needs regular monitoring and treatment. Taking control of your treatment can make you feel more in control of your life.
- Get vaccinated for influenza and pneumonia. Staying current with vaccinations can prevent flu and pneumonia from triggering asthma flare-ups.
- Identify and avoid asthma triggers. A number of outdoor allergens and irritants — ranging from pollen and mold to cold air and air pollution — can trigger asthma attacks. Find out what causes or worsens your asthma, and take steps to avoid those triggers.
-
Monitor your breathing. You may learn to recognize warning signs of an impending attack, such as slight coughing, wheezing or shortness of breath.
But because your lung function may decrease before you notice any signs or symptoms, regularly measure and record your peak airflow with a home peak flow meter. A peak flow meter measures how hard you can breathe out. Your doctor can show you how to monitor your peak flow at home.
-
Identify and treat attacks early. If you act quickly, you're less likely to have a severe attack. You also won't need as much medication to control your symptoms.
When your peak flow measurements decrease and alert you to an oncoming attack, take your medication as instructed. Also, immediately stop any activity that may have triggered the attack. If your symptoms don't improve, get medical help as directed in your action plan.
- Take your medication as prescribed. Don't change your medications without first talking to your doctor, even if your asthma seems to be improving. It's a good idea to bring your medications with you to each doctor visit. Your doctor can make sure you're using your medications correctly and taking the right dose.
- Pay attention to increasing quick-relief inhaler use. If you find yourself relying on your quick-relief inhaler, such as albuterol, your asthma isn't under control. See your doctor about adjusting your treatment.