Sept. 21, 2022
About 30% of ischemic strokes are caused by heart disease. But determining whether an individual's stroke has a cardiac etiology — and how best to manage the risk of future stroke or transient ischemic attack (TIA) — can be challenging.
Mayo Clinic's Heart Brain Clinic provides multidisciplinary expertise and a personalized approach for these complex decisions. Patients see a subspecialized stroke-cerebrovascular neurologist and an interventional cardiologist during the same half-day visit.
"That integrated consultation is an efficient means of providing multidisciplinary expertise," says Robert D. Brown Jr., M.D., M.P.H., a neurologist at Mayo Clinic in Rochester, Minnesota. "Experts work side by side — not just in the same medical center, but in the same room — on behalf of the patient. The Heart Brain Clinic is a great example of Mayo Clinic at its best."
Determining stroke etiology
Determining stroke etiology
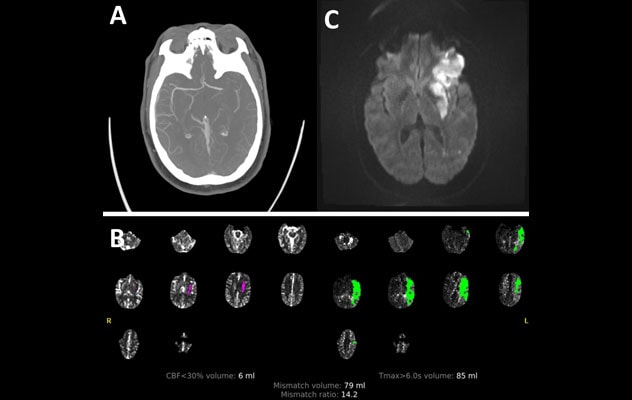
A 38-year-old woman who was previously healthy awoke with dense right hemiplegia and aphasia. A. CT angiogram showed left middle cerebral artery occlusion. B. CT perfusion showed an ischemic penumbra of potentially salvageable tissue. The patient underwent thrombolysis in cerebral infarction 2b recanalization. C. MRI of the brain at discharge showed ischemic infarct over the left inferior frontal lobe and lentiform. Head and neck angiogram showed no steno-occlusive disease, and hypercoagulable work-up was unremarkable. The patient was referred to the Heart Brain Clinic for comprehensive evaluation. Echocardiogram revealed a PFO with atrial septal aneurysm. The stroke etiology was determined to be paradoxical embolic secondary to the PFO. The patient underwent successful PFO closure.
Care focuses on determining the precise cause of an individual's stroke or TIA and whether that individual would benefit from a specific cardiac intervention to reduce the risk of future stroke.
"We commonly assess patients with atrial fibrillation, who tend to be older adults, and — at the other end of the spectrum — younger patients who have a patent foramen ovale (PFO)," says Michelle P. Lin, M.D., M.P.H., a neurologist at Mayo Clinic in Jacksonville, Florida. "Our approach is evidence-based, to decide whether an individual is a good candidate for a procedure to treat one of those conditions."
Patient-centered experience
Patients referred to the Heart Brain Clinic have generally had preliminary medical imaging, such as MRI of the brain, an assessment of their neck and brain arteries, and echocardiography. "We review the records before patients arrive, and pre-schedule any additional testing," Dr. Brown says.
Additional testing might include more-detailed echocardiography or magnetic resonance or CT angiogram if not completed already, blood tests to identify possible clotting abnormalities, and prolonged heart monitoring to assess for atrial fibrillation.
When patients arrive at Mayo Clinic, they have thorough clinical evaluations by a stroke-cerebrovascular neurologist and an interventional cardiologist. "By the end of the morning, we have recommendations in place for additional testing that may be needed to clarify the cause of stroke or TIA, and for the optimal strategy for preventing future stroke," Dr. Brown says.
For individuals with nonvalvular atrial fibrillation, the risk of stroke typically arises from clots that may form in the left atrial appendage (LAA). Anticoagulants are one treatment option.
But if long-term use of an anticoagulant isn't feasible, LAA occlusion can be an option. "The typical candidate for device-based LAA occlusion will have persistent nonvalvular atrial fibrillation, a significant risk of thromboembolism and an increased risk of bleeding related to chronic anticoagulant therapy," says Guy S. Reeder, M.D., an interventional cardiologist at Mayo Clinic's campus in Minnesota.
Federal guidelines require that patients be able to tolerate an anticoagulant for six weeks after implantation of an LAA occlusion device. "However, patients with absolute contraindications to anticoagulants have been treated with anti-platelet therapy alone post-procedure, with excellent outcomes," Dr. Reeder says. This approach is under further study.
Determining the optimal approach for managing a PFO requires similarly careful decision-making.
"PFO is extremely common in the general healthy population. The challenge lies in identifying patients who will benefit from PFO closure," says Gyanendra Kumar, M.D., a neurologist at Mayo Clinic in Phoenix/Scottsdale, Arizona.
Individuals with incidentally discovered PFOs who haven't had neurological symptoms, or who have no evidence of clinically significant right-to-left shunting, generally don't require further evaluation in the Heart Brain Clinic.
However, individuals with cryptogenic stroke who are otherwise healthy are typically considered candidates for PFO closure, particularly if they are under the age of 60. Patients over the age of 60 may be considered for the procedure as well.
Thorough neurological evaluation is essential for excluding other common causes of stroke. "On occasion, we close PFOs for patients who are slightly older if they have had a truly cryptogenic stroke but have no vascular risk factors such as high blood pressure, diabetes or abnormal cholesterol levels," Dr. Kumar says.
Stroke prevention in younger adults is an increasing concern. "While the incidence of ischemic stroke among those over the age of 65 has decreased over the past two decades, population-based studies show that the incidence is rising in young adults," Dr. Kumar says. "Having a stroke at a young age has a greater negative impact on an individual, a family and society in general. The mortality risk in this age group is also fivefold higher compared with the general population."
The feedback from patients about Heart Brain Clinic care is highly positive. "They appreciate coming to the clinic only once to see two experts across two specialties," Dr. Lin says. "Afterward, patients walk out the door knowing exactly what to expect for their care."
For more information
Refer a patient to Mayo Clinic.