May 22, 2021
Prostate cancer is the most common new cancer diagnosis in men. Men with intermediate- or high-risk prostate cancer often undergo definitive local therapy in the form of prostatectomy or radiation. In cases of a suspected local recurrence after prostatectomy, men may undergo salvage radiation. Unfortunately, a small subset of these men will develop posterior urethral stenosis. Men who have undergone combination external beam radiation and brachytherapy also are at risk. Posterior urethral stenosis can develop in approximately 10% of men with a history of these treatments.
Urosymphyseal fistula
Urosymphyseal fistula
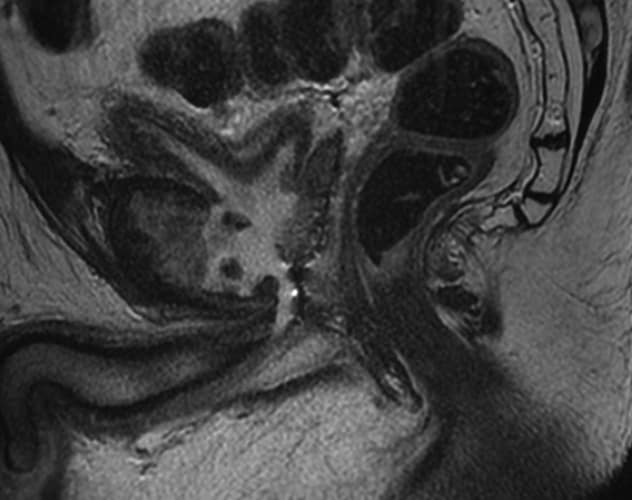
MRI images of urosymphyseal fistula in the sagittal (left) and coronal (right) planes.
Often endoscopic treatment is performed in men with posterior urethral stenosis. Repetitive or aggressive manipulation of the posterior urethra after radiation can lead to devastating sequelae. Most notably, there is a small risk of developing urosymphyseal fistula. In these cases, a direct fistula from the posterior urethra to the pubic symphyseal joint develops. Resultant progressive and recalcitrant osteomyelitis of the adjacent bone can occur. Men may present with debilitating groin pain, obstructive urinary symptoms, urinary tract infections and sepsis.
Boyd R. Viers, M.D., a reconstructive urologist at Mayo Clinic in Rochester, Minnesota, led a team that evaluated the natural history of 25 men with urosymphyseal fistula who went on to undergo bone resection and urinary reconstruction. Study results were published in BJU International in 2021.
Jack R. Andrews, M.D., a chief resident at Mayo Clinic in Rochester, Minnesota, a Mayo Clinic scholar at Mayo Clinic in Phoenix/Scottsdale, Arizona, and the first author of the study, notes: "We found that patients often presented with symptoms of a urosymphyseal fistula after a pretty long interval. In our series, the median time to diagnosis after radiation was 11 years."
The authors discovered other interesting findings as part of their analysis, including:
- Nearly all patients presented with debilitating groin pain with ambulation (24 of 25; 96%) and were diagnosed with pelvic MRI.
- Of the 25 patients, 76% had endoscopic urethral manipulation within six months preceding diagnosis of urosymphyseal fistula.
- Discordance between preoperative urine and intraoperative bone cultures was present in most men (95%).
- While 48% of patients experienced complications within 90 days following urinary reconstruction, nearly all (96%) reported complete resolution of symptoms and restoration of baseline performance status.
Dr. Viers summarizes: "Ultimately, early recognition of those men who've undergone radiation and are at risk for urosymphyseal fistula and avoidance of repetitive urethral manipulation for posterior urethral obstruction is the first critical step. Urologists should have a high index of clinical suspicion in those patients presenting with debilitating groin pain with ambulation. Pelvic MRI is the diagnostic study of choice to confirm the presence of urosymphyseal fistula.
"Conservative management in this population ultimately fails due to lack of fistula control, inability to accurately target antimicrobial therapy due to discordant bacterial growth, and poor tissue penetration in the setting of irradiated, poorly vascularized tissue. We believe that a multidisciplinary reconstructive approach provides durable restoration of quality of life in appropriately selected men."
For more information
Andrews JR, et al. Pubectomy and urinary reconstruction provides definitive treatment of urosymphyseal fistula following prostate cancer treatment. BJU International. In press.