Oct. 06, 2017
Fractures of the acetabulum are challenging orthopedic injuries to repair, at times leaving multiple small fragments of fractured bone and cartilage. Compounded by the location in a region challenging in which to work and fraught with risk, these "puzzle pieces" must be brought back together to restore hip function and mobility.
The acetabulum, commonly thought of as the socket of the ball-and-socket hip joint, may break in one of 10 different pattern classifications discussed in the January 2014 issue of Clinical Orthopaedics and Related Research "Classifications in Brief".
Relative to hip fracture, acetabular fracture is uncommon. These fractures occur in two distinct patient populations:
- In younger patients, high-energy injuries cause the break, such as motor vehicle or bike accidents, or falls from significant height.
- In older patients with osteoporosis, low-energy injuries such as falls from standing height prompt the fracture.
Patients' pain levels vary widely and are related to the injury pattern and mechanism of injury.
Risks with acetabular fracture
This fracture puts patients at considerable risk of developing post-traumatic arthritis, which may result in the need for hip replacement. Post-traumatic arthritis occurs due to damage to the articular surface of either the acetabulum or femoral head. Another potential complication with acetabular fracture is avascular necrosis, in which the blood supply to the femoral head is sufficiently damaged or stretched from dislocation that the bone subsequently dies and collapses, resulting in hip pain.
"The acetabulum is an articular surface — it articulates with the femoral head," says Stephen (Andy) A. Sems, M.D., an orthopedic trauma surgeon at Mayo Clinic's campus in Rochester, Minnesota. "If the acetabulum is not well-reduced or maligned — or sometimes even if the surgeon is able to achieve the reduction and the alignment — the cartilage coating the joints has been badly damaged and degenerates, which is arthritis. It just wears out — the cartilage wears away and you get the situation of a painful degenerative joint."
Acetabular fractures are commonly associated with multiple other injuries, such as to the abdomen, chest or head. With isolated acetabular fracture, the risk of shock is low, but concomitant injuries must be identified and treated appropriately.
Surgical treatment of acetabular fracture is complex and can result in complications and poor outcomes. While the infection risk is similar to that of other hip procedures, body mass index (BMI) is a predictor of infection and complications of operative treatment.
"There are a lot of theories as to why BMI is associated with infection, but it's been shown in a few different studies in pelvic ring injuries and acetabular fractures that higher BMI is associated with complications," says Dr. Sems, noting he and colleagues published on this topic in the May 2010 Journal of Orthopaedic Trauma, as did Karunakar and colleagues in the July 2005 issue of The Journal of Bone and Joint Surgery, American Volume.
Orthopedic surgeons who work with acetabular fractures and their patients with elevated BMI have to understand the high risks with surgery and make wise decisions based on the risks, according to Dr. Sems.
"In some patients with predictably poor outcome, we proceed right to hip replacement at Mayo Clinic," he says.
Fracture management
When patients with suspected acetabular fracture arrive at any hospital, the first order of business is to determine if the hip is reduced or dislocated. If dislocated, providers should perform urgent closed reduction prior to any transfers, as this procedure is crucial to preventing future complications.
"You can imagine that transferring someone with a dislocated hip would be incredibly painful for that patient, and it also delays the time to get the hip reduced, which is associated with a worse outcome — avascular necrosis," says Dr. Sems.
If the hip is unable to be reduced or appears widely displaced, consult with a higher level trauma center for transfer.
Physical exams for patients who have potentially suffered this injury are minimal, usually differentiating between acetabular or hip fracture.
"There's not much of a physical exam — you can check the ability for the ankle or toes to dorsiflex; and check the sciatic nerve, particularly the peroneal branch; and check sensation in the superficial peroneal and deep peroneal nerve distributions," says Dr. Sems, indicating nerve status should be documented. "But there is not much that's going to be able to distinguish this from a hip fracture."
Preoperative 3-D reconstruction CT scans showing acetabular injury
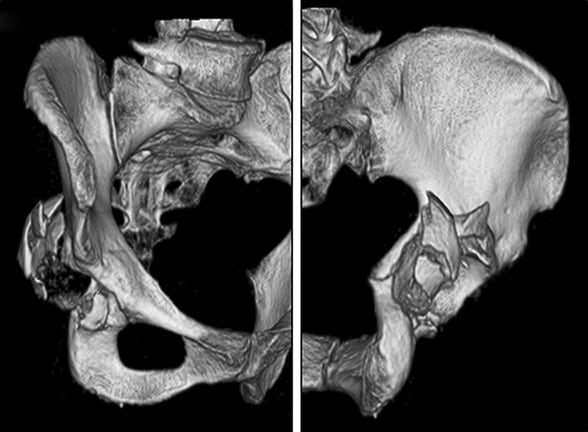
Preoperative 3-D reconstruction CT scans showing acetabular injury
Preoperative 3-D reconstruction CT scan showing the magnitude of the acetabular injury. Image reprinted with permission from The Bone & Joint Journal.
X-rays, including anteroposterior pelvis and oblique X-rays of the pelvis, are mandatory with suspected acetabular fracture, and CT scans are commonly performed, as well. If the acetabular fracture is the only serious injury, hospitals should take the time for imaging prior to transfer, once the patient is stabilized. In multi-injured patients, transfer should not be delayed for imaging.
Dr. Sems suggests consulting with a Level I trauma center, where specialists can review films and advise regarding next steps in the patient's care. Not every patient with an acetabular fracture needs to be transferred to a higher level of care. "Have an orthopedic trauma surgeon at Mayo Clinic look at your images prior to transfer, particularly in low-energy injuries in older adult patients — these patients generally are not emergencies or even urgencies," says Dr. Sems. "There's plenty of time with those. This is nothing we're doing in the middle of the night."
Cases where the acetabulum is widely displaced and the patient is significantly more unstable require more aggressive treatment, often surgery. If surgery is needed to repair an acetabular fracture, patients should be transferred to a higher level of care.
Surgical repair
Dr. Sems recommends acetabular fractures requiring surgery be performed at a Level I trauma center, as this type of surgery necessitates a hospital where it is done frequently.
"These outcomes are marginal to begin with, and the best outcomes are likely associated with more experience and repetition," says Dr. Sems. "There is a long learning curve with acetabular surgery. With experience tends to come improved reductions, and excellent reductions are one of the biggest predictors of good outcomes."
Generally, for acetabular fracture in patients with hip dislocation or wide displacement, surgery is performed within one week of injury.
While awaiting surgery, some patients are placed in traction to preserve the hip joint and keep the hip reduced. For those too ill to undergo an operation, not yet resuscitated appropriately or where multiple other injuries are present, a longer wait for surgery may be warranted.
Surgical recovery involves several months, with most patients placed on weight-bearing precautions for the first three months, followed by a process of gradual mobilization. Some — though not all — patients' recoveries progress so well they are able to return to the ball field or basketball court.
"Our goal is to have a good functional return where patients can perform the activities of daily living and do most of the activities they were performing prior to this injury without debilitating pain," says Dr. Sems.
For more information
Alton TB, et al. Classifications in brief: Letournel classification for acetabular fractures. Clinical Orthopaedics and Related Research. 2014;472:35.
Sems SA, et al. Elevated body mass index increases early complications of surgical treatment of pelvic ring injuries. Journal of Orthopaedic Trauma. 2010;24:309.
Karunakar MA, et al. Body mass index as a predictor of complications after operative treatment of acetabular fractures. The Journal of Bone & Joint Surgery, American Volume. 2005;87:1498.
Sierra RJ, et al. Acetabular fractures: The role of total hip replacement. The Bone & Joint Journal. 2013;95-B(11 suppl A):11.