Aug. 18, 2018
Macular degeneration is a class of diseases characterized by the loss of central, high-acuity vision. In most, if not all, cases, macular degeneration is the result of retinal pigment epithelium (RPE) dysfunction.
RPE transplantation was a subject of much research as a treatment for macular degeneration starting in the 1980s. The discovery of processes for the differentiation of embryonic stem cells to RPE has renewed interest in RPE transplantation. That interest has been further revitalized by the discovery of methods to reprogram cells into a pluripotent state. Induced pluripotent stem cells (iPSC) can be generated from adult cells and thus are free of the ethical and legal issues that surround the use of embryonic stem cells. Another advantage of iPSC is that they can be generated from the patient in which the cells are to be re-transplanted.
Stem cell-derived RPE cell transplantation is currently in phase I clinical trials for macular degeneration. A major obstacle in these studies is the need to deliver the RPE as living, flat sheets without folding and clumping of the monolayer, or leaving behind foreign materials in the retina. Jarel K. Gandhi, Ph.D., and a research team led by Alan D. Marmorstein, Ph.D., in Ophthalmology Research at Mayo Clinic's campus in Rochester, Minnesota, investigated the suitability of using hydrogels made from human blood-derived proteins for RPE transplant. Study results were published in Acta Biomaterialia in 2018.
Fibrin hydrogels as a scaffold
To overcome the issue of folding and clumping of the monolayer, the researchers investigated the use of hydrogels generated from human fibrin as a scaffold for RPE transplantation. Fibrin is a cross-linking fibrillar network formed spontaneously after the activation of fibrinogen. Fibrin forms the scaffold of the blood clot that physiologically occurs during wound healing, and has a well-established cascade of activation, formation, degradation and clearance.
Implant of iPSC-RPE cultured on a fibrin hydrogel
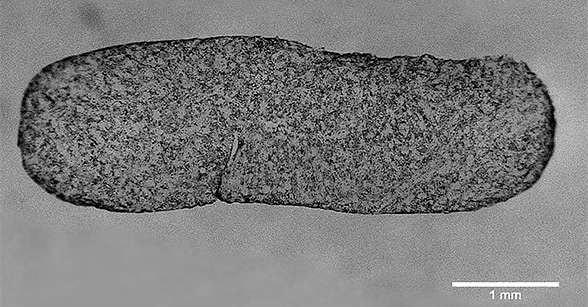
Implant of iPSC-RPE cultured on a fibrin hydrogel
The implant of iPSC-RPE cultured on a fibrin hydrogel depicted is a 5.0-by-1.5-mm rounded rectangle, with a thickness of 0.2 mm.
To test the suitability of fibrin as a substrate for RPE transplantation, the research team produced a variety of fibrin hydrogels by varying the concentrations of fibrinogen and thrombin to form a thin rigid hydrogel with defined parameters for degradation in the scale of hours in vitro. Subsequently, the optimized conditions were utilized to produce fibrin gels on which the researchers cultured iPSC-RPE, forming well-differentiated monolayers.
"This study demonstrates the ability to generate large surfaces of iPSC-RPE on fibrin hydrogels, such as a 60-mm-diameter (28-cm2) circle. Generating large surfaces out of a single gel, as demonstrated, has tremendous benefits for clinical applications," says Dr. Gandhi. "Over 250 implants (1.5 mm by 5 mm) can be punched out from a single 60-mm-diameter gel. This enables quality testing on the same batch of cells that would be used for the clinical trial. This also provides a surgeon with many options to select which region of the culture to implant. It allows for the prospect of implanting multiple sheets to cover a larger area, theoretically the entire 5-mm-diameter macula with as little as three implants. Or multiple implants can be used to target peripheral RPE replacement in various locations, in diseases of the peripheral retina. In addition, it has the potential to reduce the overall cost of the transplant."
Finally, the researchers degraded the fibrin support in vitro, and the effects of this degradation on the RPE monolayer were assessed. The RPE remained viable and pigmented. "While many groups have investigated a large variety of hydrogels for RPE culture and support, fibrin has not been reported for this purpose previously," says Dr. Marmorstein. "We suspect that a key difficulty encountered by others in the use of fibrin may have been the tendency of the RPE to degrade fibrin on its own.
"Stem cell-derived RPE cells require months to differentiate fully in culture, but we found that RPE degraded fibrin hydrogels in a matter of days. As such, a key finding of our study is the use of protease inhibitors, such as aprotinin, to preserve fibrin during RPE culture. This preserves the gel throughout the differentiation process, but allows it to be degraded when the protease inhibitors are washed out. Again, even without the addition of exogenous fibrinolytic enzymes, the RPE is able to degrade the fibrin gel rapidly."
"Our data suggest that fibrin hydrogels hold great potential for use as a long-lived scaffold for the differentiation of RPE from stem cells that can then be degraded under controlled circumstances following delivery to the subretinal space," says Dr. Gandhi. "Fibrin hydrogels offer a promising solution to transplant RPE for patients with macular degeneration."
For more information
Gandhi JK, et al. Fibrin hydrogels as a xenofree and rapidly degradable support for transplantation of retinal pigment epithelium monolayers. Acta Biomaterialia. 2018;67:134.