Nov. 25, 2015
Osteoporosis is widely understood to be associated with low bone mass. Matthew T. Drake, M.D., Ph.D., an endocrinology consultant at Mayo Clinic's campus in Rochester, Minnesota, says: "It is less well-appreciated, however, that this loss of bone tissue is also associated with significant deterioration of the skeletal microarchitecture. Collectively, these changes in both bone mass and microstructure lead to compromised bone strength and increased fracture risk.
"Further, while the World Health Organization has defined osteoporosis as bone mineral density (BMD) at the hip or spine less than or equal to 2.5 standard deviations below the young normal mean, more fractures occur in patients with osteopenia than osteoporosis due to the fact that osteopenia is far more prevalent in the population."
Whereas bone mass declines with aging, so too does bone quality. Dr. Drake explains: "It has been clearly shown that age predicts bone fragility and fracture risk independent of areal BMD determined by dual energy X-ray absorptiometry (DXA) imaging. Thus, for the same areal BMD, a 70-year-old woman has a tenfold or greater risk of fragility fracture when compared with a 30-year-old woman. Importantly, this areal BMD-independent effect of aging has been attributed to decreased bone quality."
Potential sources of this age-associated decline in bone quality include:
- Trabecular thinning, perforation or loss of connectivity
- Cortical thinning or increases in porosity
- Changes in bone material properties such as the composition and degree of collagen cross-linking
Historically, the gold standard method for assessment of bone microarchitectural properties has involved obtaining a bone biopsy. However, bone biopsies are invasive, require sedation, are typically obtained only from the iliac crest (a non-weight-bearing site that is unlikely to fracture) and suffer from an inability to accurately assess longitudinal changes, as biopsy sites are different.
Likewise, standard DXA imaging has its own limitations, due to its measurement of bone mineral content over a projected bone area to provide an areal BMD. These limitations stem from the inability of DXA imaging to differentiate cortical from trabecular bone, its provision of a 2-D (areal) measurement of a 3-D structure, and its tendency to underestimate BMD of smaller bones and overestimate BMD of larger bones.
Dr. Drake comments: "The recent development of high-resolution peripheral quantitative computerized tomography (HRpQCT) imaging has overcome many of the above limitations. HRpQCT imaging allows for noninvasive bone biopsy at the distal radius and tibia, providing in vivo assessment of bone geometry, true 3-D (volumetric) BMD and microarchitecture at extremely high resolution (60 to 82 μm).
"Further, HRpQCT imaging allows for the construction of microfinite element models of bone strength that can be used to estimate fracture risk. HRpQCT imaging permits measurement of both trabecular (bone fraction, number, thickness, separation, area and volumetric BMD) and cortical (thickness, volumetric BMD, area, endosteal and periosteal circumference) parameters and exposes subjects to minimal radiation.
"A recent example demonstrating the utility of HRpQCT imaging involves our work at Mayo Clinic demonstrating the skeletal significance that occurs in patients with monoclonal gammopathy of undetermined significance (MGUS). Although fracture rates are substantially increased in patients with MGUS, whether bone loss occurs in MGUS has remained unclear, with most studies demonstrating no decreases in areal BMD by DXA imaging.
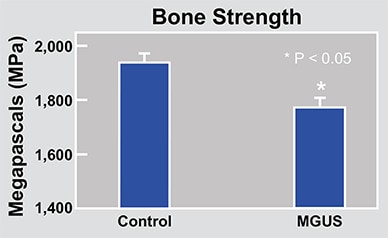
"To address this directly, we studied 50 subjects with MGUS (mean age of 70 years) by HRpQCT imaging and compared them with 100 control subjects matched for age, sex and body mass index. Whereas areal BMD as assessed by DXA imaging was not different between the groups, HRpQCT imaging demonstrated a highly significant decrease of greater than 10 percent in volumetric BMD as well as significant decreases in trabecular and cortical bone parameters.
"Together, these changes were associated with significant decreases in bone strength, strongly suggesting that these alterations in bone microstructure are likely important determinants of the increased fracture risk seen in patients with MGUS."
Assessment of bone microarchitecture
Assessment of bone microarchitecture
A Mayo Clinic research protocol allows assessment of bone microarchitecture based on HRpQCT imaging.
Determination of trabecular bone score
Determination of trabecular bone score
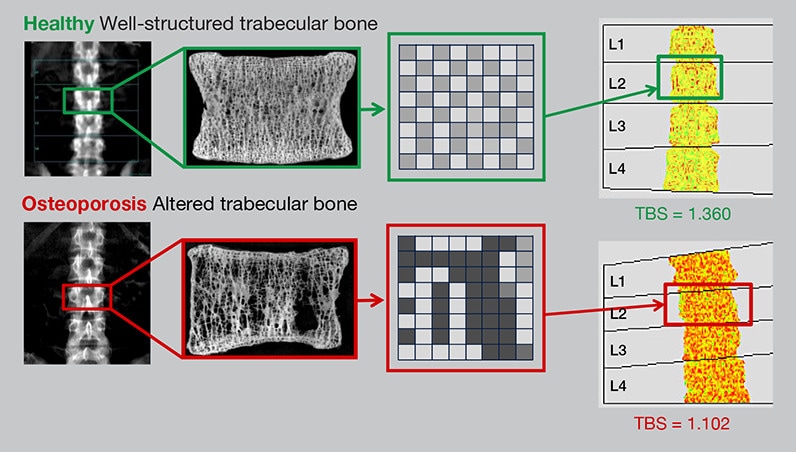
Trabecular bone score (TBS) uses standard lumbar spine DXA imaging to assess bone texture inhomogeneity (that is, the number of filled versus unfilled voxels) in order to gauge bone quality and fracture risk.
HRpQCT imaging of bone in control and patient with MGUS
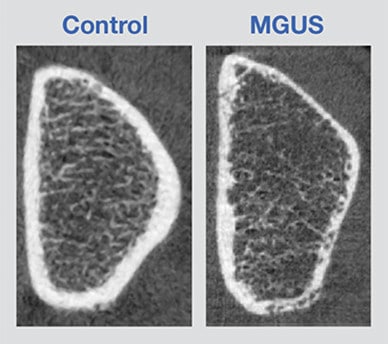
HRpQCT imaging of bone in control and patient with MGUS
Patients with MGUS have increased cortical porosity and decreased bone strength as measured by HRpQCT imaging.
It is important to note that HRpQCT imaging remains a research investigative tool that has not yet received regulatory approval for clinical use, although at Mayo Clinic there is an active research protocol that allows assessment of bone microarchitecture by HRpQCT imaging in patients with a history of fracture despite normal or near-normal DXA-determined areal BMD.
Whereas access to HRpQCT imaging remains limited, a novel method for assessing bone quality and fracture risk at the lumbar spine has recently been developed. Dr. Drake explains: "Termed trabecular bone score (TBS), this method uses standard DXA spine images to measure texture inhomogeneity — that is, how well-structured or poorly structured the trabecular bone appears when assessed as individual voxels.
"To do so, TBS utilizes a software program installed on a standard DXA computer to provide an index of bone microarchitecture based upon the assessed trabecular texture. TBS does not require additional scan time or radiation exposure. Importantly, TBS has recently been shown to independently predict fracture risk, to complement standard areal BMD imaging in patients with low bone mass, and to relate better to fracture risk than does areal BMD in patients with secondary osteoporosis.
"TBS has recently been integrated into international guidelines from the International Osteoporosis Foundation and the International Society for Clinical Densitometry as a validated risk factor for fracture. Further, the FRAX risk assessment tool has recently added a new feature that allows calculated FRAX scores to be adjusted for TBS. As with DXA imaging, TBS can be used at the time of treatment initiation as well as at subsequent visits, and can even be performed retrospectively on archived spine DXA images to assess previous longitudinal changes in lumbar spine bone quality.
"Finally, it should be noted that at present TBS can only be used to assess bone quality and fracture risk at the spine, although future studies to better understand its clinical utility at the hip appear likely."