Aug. 04, 2020
Pediatric brain tumors require specialized treatment that differs from the regimens used in adults. Mayo Clinic's Pediatric Brain Tumor Clinic employs a multidisciplinary approach focused on the particular needs of children while drawing on the broad resources of a major tertiary center.
Part of the Mayo Clinic Children's Center, the Pediatric Brain Tumor Clinic brings together pediatric specialists in neuro-oncology, neurology, neurosurgery, neuroradiology, radiation oncology and neuropathology. Patients referred to Mayo for pediatric brain tumors can often be seen the next day.
"Our multidisciplinary team can be put into place very quickly," says Jonathan D. Schwartz, D.O., M.P.H., a pediatric neuro-oncologist at the Mayo Clinic Children's Center in Rochester, Minnesota. "We communicate with one another so everyone is on the same page, and families can quickly get a detailed diagnosis and a treatment plan."
State-of-the-art imaging, such as 7-tesla MRI, facilitates the planning of surgical and radiation procedures. For complex tumor resections, Mayo's pediatric neurosurgeons collaborate with colleagues in adult neurosurgery, otorhinolaryngology/ENT and neuro-ophthalmology.
"Depending on the case, we might work for example with skull base or peripheral nerve surgeons who are recognized as leaders in their field," says David J. Daniels, M.D., Ph.D., a pediatric neurosurgeon at Mayo's campus in Minnesota. "This collaboration allows us to manage cases that can't be easily done elsewhere."
To safeguard the developing pediatric brain, Mayo Clinic uses proton beam therapy to deliver targeted radiation. "Children who get proton treatment have fewer side effects in terms of IQ changes, cognitive development, growth, and endocrine development and hormonal problems than children who have traditional radiotherapy," says Nadia N. Laack, M.D., chair of Radiation Oncology in the Children's Center at Mayo's campus in Minnesota.
As a large-volume center, Mayo Clinic is also committed to clinical trials and research aimed at providing more-targeted treatments. "Right now, the number of treatment options for pediatric brain tumors is limited. It's critical that we develop novel therapeutics and treatment options, to maximize treatment and minimize long-term consequences for children," Dr. Schwartz says.
Precision targeting of tumors
Pediatric brain tumors pose unique challenges and require highly specialized expertise. "The entire resources of Mayo Clinic's strong neuro-oncology program are available to our pediatric patients," Dr. Laack says.
In addition to 7-tesla MRI, Mayo is studying the nuclear medicine marker known as fluorine F18 fluorodopa-positron emission tomography to delineate precise targets for radiation treatment. Diffusion tensor imaging (DTI) tractography may be used to guide tumor resection.
"DTI allows us to really understand the relationship between the tumor and eloquent areas of the brain and corticospinal tract," Dr. Daniels says.
Tumor resection is further enhanced by Mayo's routine collaboration among surgical specialists. Dr. Daniels cites a recent case in which the pediatric patient's tumor extended from the brain through one eye to the face. The surgical team included a pediatric neurosurgeon, an ENT surgeon and an eye surgeon. "None of us could have done that case alone," Dr. Daniels says.
Radiation therapy is directed at maximizing tumor treatment while minimizing damage to surrounding tissue. Gamma Knife radiosurgery is used in select pediatric patients with benign brain tumors as well as metastatic disease. For primary brain cancer, Mayo Clinic has utilized proton beam therapy for about five years.
"There are increasing numbers of reports with long-term follow-up data demonstrating that children receiving proton radiation for brain tumors, such as medulloblastoma, show minimal declines in their cognitive development," Dr. Laack says. "That contrasts with traditional radiotherapy, where we generally see a steady decline in development after treatment."
That reduced toxicity can be achieved without compromising tumor outcomes. As described in the Sept. 1, 2019, issue of the International Journal of Radiation Oncology, the two-year survival rate for children with brain tumors treated with pencil beam scanning therapy at Mayo Clinic is 93%.
Recommendations concerning the optimal approach to an individual's disease are made at weekly meetings of Mayo's multidisciplinary pediatric brain tumor board. "We discuss our own patients' cases, as well as outside cases, to determine if there is an approach that might help," Dr. Laack says. "Our model of care ensures that each patient has a thorough case review, and potentially access to new radiation studies or techniques or new surgical options."
Una resonancia magnética preoperatoria muestra un ependimoma de alto grado
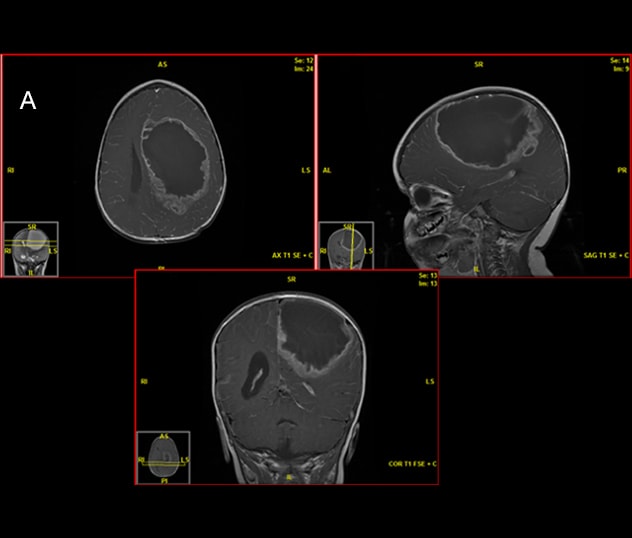
Una resonancia magnética preoperatoria muestra un ependimoma de alto grado
Una resonancia magnética preoperatoria muestra un ependimoma de alto grado en un paciente de 18 meses.
La histopatología muestra un ependimoma anaplásico, con una secuenciación posterior y un microarreglo cromosómico que demuestra la fusión de RELA
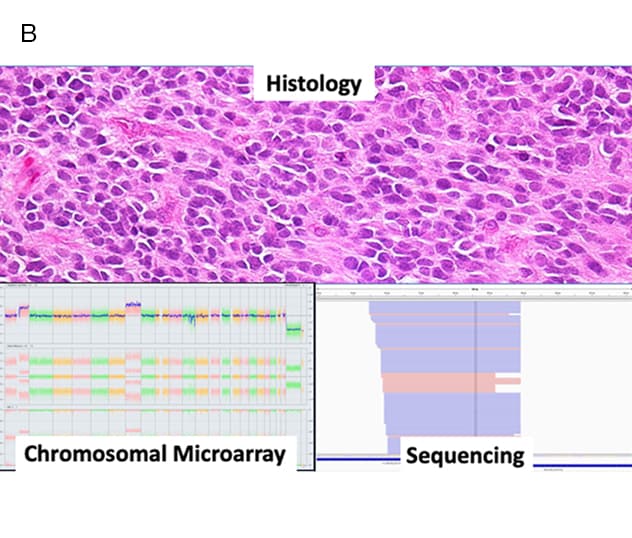
La histopatología muestra un ependimoma anaplásico, con una secuenciación posterior y un microarreglo cromosómico que demuestra la fusión de RELA
La histopatología muestra un ependimoma anaplásico, con una secuenciación posterior y un microarreglo cromosómico que demuestra la fusión de RELA, lo que indica un tumor agresivo y subraya la conveniencia de la radioterapia.
La terapia de rayos de protones se utiliza para evitar la toxicidad en el tejido cerebral circundante
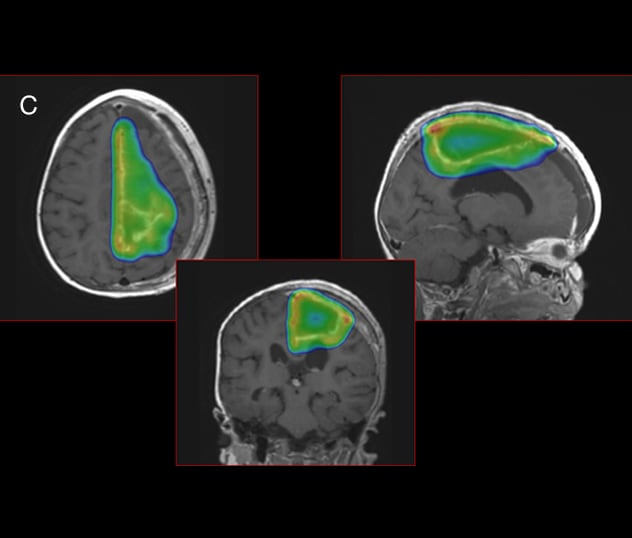
La terapia de rayos de protones se utiliza para evitar la toxicidad en el tejido cerebral circundante
Para evitar la toxicidad en el tejido cerebral circundante, Mayo usó la terapia de rayos de protones. La nube de dosis de protones, mostrada en color, demuestra la estrecha conformidad de la terapia de protones con el tumor del niño.
The tumor board also incorporates Mayo's expertise in neuropathology. The integration of comprehensive genetic testing, such as neuro-oncology-specific next-generation sequencing and chromosomal microarray analysis, can provide more-detailed information about an individual child's brain tumor. "That's especially helpful for tailoring therapy directly to the patient if a tumor has a risk of recurrence," Dr. Schwartz says.
Advancing personalized care through research
As a member of consortia including the Children's Oncology Group and the National Comprehensive Cancer Network, Mayo Clinic strives to give select pediatric patients access to clinical trials. "Our tumor board evaluates if a particular clinical trial might benefit children and if we can safely advocate to open that trial to younger ages," Dr. Laack says.
Mayo is also active in developing its own clinical studies. One current investigation is a detailed look at how radiation affects children's cognitive functioning. Specifically, the researchers are evaluating how tumor location and radiation dose correlate with subsequent problems with memory, attention, vision, motor skills, and spatial and executive functioning.
"We're trying to understand each child's individual strengths and weaknesses, and adjust our radiation dosing based on that," Dr. Laack says.
A separate pilot clinical study is evaluating the feasibility of using memantine to reduce cognitive impairment in children who receive radiation therapy. Mayo investigators previously conducted a similar successful study in adults.
In addition to testing existing medications, Mayo is working to develop new therapies. The Experimental Drug and Therapeutics for Pediatric Brain Tumor Laboratory, led by Dr. Daniels, studies the physical properties of various medications and how they might be used against pediatric brain tumor. Dr. Daniels hopes eventually to test some of these medications in the setting of convention-enhanced delivery.
"Delivering a drug directly to the brain tumor bypasses the blood-brain barrier," he says. "We are keenly interested in trying to understand which drugs might be optimal for treating tumors in this way."
One potential disease target is diffuse intrinsic pontine glioma (DIPG), a rare tumor that typically occurs in young children and is fatal within a year. "In our lab studies, we've found that alisertib — a selective Aurora A Kinase inhibitor — is quite effective on these tumors," Dr. Daniels says. "In addition, we've shown that alisertib enhances the activity of radiation, which is the only therapy that has ever been found to benefit kids with DIPG."
In both research and treatment, Mayo's goal is a personalized medicine approach. The key is greater insight into individual tumor makeup.
"With that knowledge, we'll better understand the consequences and side effects of treatment. We will be much more precise about how an individual's tumor should be approached," Dr. Laack says. "We are working toward a future where each individual child has fewer side effects and the best chance of cure."
For more information
Rongthong W, et al. Effect of prospective use of radiobiologic effect (RBE) modeling in treatment planning on magnetic resonance imaging (MRI) radiation related changes (RRC) in pediatric patients with brain tumors treated with pencil beam scanning proton therapy (PBS). International Journal of Radiation Oncology. 2019;105:E628.