Aug. 21, 2020
Personal de cardiooncología en la sede de Mayo Clinic en Phoenix/Scottsdale, Arizona
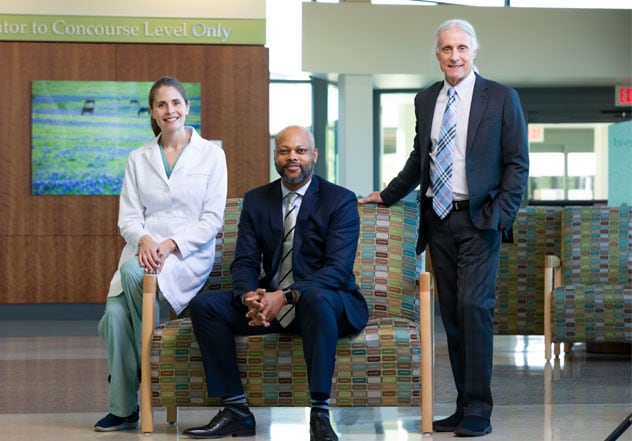
Personal de cardiooncología en la sede de Mayo Clinic en Phoenix/Scottsdale, Arizona
Clínica Mayo en Arizona: Carolyn M. Larsen, MD, Enfermedades Cardiovasculares; Brian W. Hardaway, MD, Enfermedades Cardiovasculares; y Donald W. Northfelt, MD, Hematología y Oncología Médica. Sin foto: Reza Arsanjani, MD, enfermedades cardiovasculares.
El personal de cardiooncología del campus de Mayo Clinic en Rochester, Minnesota

El personal de cardiooncología del campus de Mayo Clinic en Rochester, Minnesota
Mayo Clinic en Minnesota (en el sentido de las agujas del reloj desde la izquierda): Grace Lin, M.D., Insuficiencia Circulatoria; Hector R. Villarraga, M.D., Ecografía Cardiovascular; Naveen L. Pereira, M.D., Insuficiencia Circulatoria; Martin G. Rodriguez-Porcel, M.D., Enfermedad Cardíaca Isquémica y Cuidados Críticos; S. Allen Luis, M.B.B.S., Ecografía Cardiovascular; Paul M. McKie, M.D., Cardiología Integral; Joerg Herrmann, M.D., Enfermedad Cardíaca Isquémica y Cuidados Críticos.
Personal de cardiooncología en la sede de Mayo Clinic en Jacksonville, Florida

Personal de cardiooncología en la sede de Mayo Clinic en Jacksonville, Florida
Mayo Clinic en Florida: Jordan (Chris) C. Ray, MD y Carolyn Landolfo, MD, ambos en Medicina Cardiovascular.
In the last 15 years, the number of cancer drugs has expanded dramatically — a huge boon to cancer patients, who are surviving in record numbers. More than 16 million people have survived cancer in the U.S. alone — a number predicted to be 19 million by 2024 and 30 million worldwide. The success in treating cancer, however, is tinged by the negative effects some of the drug and radiation therapies have on heart and vascular function.
The medical community became aware of cardiac toxicity from oncology drugs in the 1970s, when many patients who were treated with high doses of doxorubicin developed heart failure. The awareness heightened in the early 2000s when anti-HER2 breast cancer therapy with trastuzumab, anti-angiogenic anticancer therapy with bortezomib and other new cancer treatments with cardiovascular toxicity potential entered clinical practice.
"We've seen a 70% increase in new cancer therapies in recent years, and many of them are tested only in phase I and II clinical trials," says Joerg Herrmann, M.D., a cardiologist at Mayo Clinic, Rochester, Minnesota. "With less vigorous testing, it's no surprise that we see unanticipated side effects. The cancer treatment field is moving so fast that many physicians have trouble keeping up with the changes, including side effects. We don't want the cancer survivors of today to become the heart disease patients of tomorrow." Mayo Clinic established cardio-oncology clinics on all three of its campuses to provide expertise for patients who will have cancer treatment, including preventing, monitoring and managing cardiovascular toxicity. This formal collaboration between cardiology and hematology/oncology is recognized as the optimal practice model to provide integrated care to patients with cancer.
Mayo Clinic is a pioneer and leader in cardio-oncology. Donald W. Northfelt, M.D., a medical oncologist at Mayo Clinic in Phoenix, Arizona, helped to establish Mayo's first cardio-oncology clinic on the Arizona campus in 2011. Dr. Herrmann helped to establish cardio-oncology on the Rochester campus and published a textbook on the topic in 2016, putting Mayo Clinic on the national map in this field. Each February, Mayo Clinic offers a well-regarded continuing medical education course, Cardio-Oncology: Putting Principles into Action in Your Practice, in Arizona. "In the past, medical institutions lacked a clear and firm connection between oncologists and cardiologists to manage cardiovascular complications of cancer and cancer therapies," says Dr. Northfelt. "At Mayo Clinic, that's no longer the case. The emergence of cardio-oncology as a distinct practice ensures we look at patients broadly from the perspective of their cardiovascular health including disease- and treatment-associated risks, not simply as cancer patients."
Oncologists refer adult and pediatric patients to cardiologists in the Mayo Clinic Cardio-Oncology Clinic with the aim of:
- Identifying at-risk patients at diagnosis, including those with existing cardiovascular disease, those at particular risk of cardiovascular disease and those whose recommended cancer therapy may pose risks
- Discussing cancer treatment options from the cardiovascular and oncologic perspectives
- Recommending preventive strategies such as diet, exercise and cardio-protective agents to minimize risk for patients at risk of heart disease
- Monitoring and treating potential cardiovascular complications before, during and after the patient's treatment
- Successfully treating the cancer while minimizing cardiotoxicity and other collateral damage
- Encouraging at-risk patients to be monitored and to manage cardiovascular risks throughout their lives
Dr. Northfelt says preventive strategies aren't as advanced as he'd like, but that presents opportunities for research. "We can check heart function testing before and during treatment, and mitigate cardiovascular side effects with drug choice and dose, drug combinations, and timing of therapy. We may want a patient to take 'the best drug' as a first choice, but if it's contraindicated by a heart condition or another factor, we can recommend another drug. We must weigh the benefit to the patient with the risk of harm from the treatment, and involve the patient in that conversation. In the meantime, we're investigating ways to protect the heart while allowing protective cancer care to occur."
Dr. Herrmann is leading the Trastuzumab Cardiomyopathy Therapeutic Intervention With Carvedilol (TACTIC) study, a five-year National Cancer Institute clinical trial with patients with breast cancer who are receiving trastuzumab-based HER2-directed therapy. These patients are at risk of heart function decline or heart failure symptoms. The study aims to determine if a cardiovascular protective strategy, such as a beta-blocker, could help when patients show significant heart function decline or subtle early signs of heart injury, or preventively before beginning therapy with trastuzumab.
"The very topic and field of cardio-oncology will remain an important aspect in the care of cancer patients in the future — this is in view of the aging of the population, considering that aging is an important risk factor for heart diseases and cancer," says Dr. Herrmann. "The toxicity spectrum of cancer drugs continues to evolve, often with unexpected side effects, as those seen with the recently emerging class of immune therapies — mainly immune checkpoint inhibitors, which are used and tested in an exponential manner in a number of cancer subtypes. For this reason, there is and remains a need for cardio-oncology collaboration and expertise now and then."
Highest risk of CV side effects
Conditions and treatments that may be associated with cardiovascular side effects ranging from hypertension to heart failure include:
- Breast cancer — left breast radiation and drug therapies
- Hodgkin's disease — radiation and drug therapies
- Non-Hodgkin's lymphoma in the chest — radiation and drug therapies
- Lung cancer — radiation and drug therapy
- Acute leukemia in children — drug therapy
- Multiple myeloma and kidney cancer — drug therapy
- Lymphoma — drug therapy
- Pancreatic cancer — the disease itself