Breast cancer types: What your type means
Not all breast cancers are the same. Understand what type of breast cancer you have and how it differs from other types of breast cancer.
By Mayo Clinic Staff
Once you've been diagnosed with breast cancer, your doctor will review your pathology report and the results of any imaging tests to understand the specifics of your tumor.
Using a tissue sample from your breast biopsy or using your tumor if you've already undergone surgery, your medical team determines your breast cancer type. This information helps your doctor decide which treatment options are most appropriate for you.
Here's what's used to determine your breast cancer type.
In what part of the breast did your cancer begin?
Breast anatomy
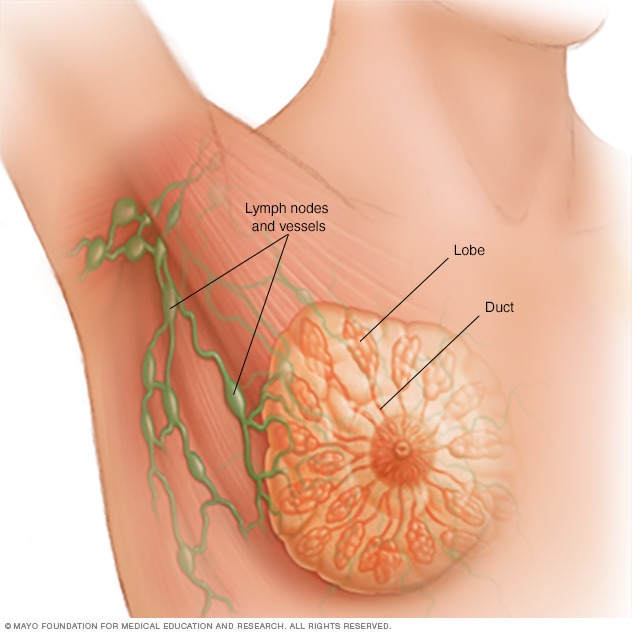
Breast anatomy
Each breast contains 15 to 20 lobes of glandular tissue, arranged like the petals of a daisy. The lobes are further divided into smaller lobules that produce milk for breastfeeding. Small tubes, called ducts, conduct the milk to a reservoir that lies just beneath your nipple.
The type of tissue where your breast cancer arises determines how the cancer behaves and what treatments are most effective. Parts of the breast where cancer begins include:
-
Milk ducts. Ductal carcinoma is the most common type of breast cancer. This type of cancer forms in the lining of a milk duct within your breast. The ducts carry breast milk from the lobules, where it's made, to the nipple.
Ductal carcinoma can remain within the ducts as a noninvasive cancer (ductal carcinoma in situ), or it can break out of the ducts (invasive ductal carcinoma).
- Milk-producing lobules. Lobular carcinoma starts in the lobules of the breast, where breast milk is produced. When it breaks out of the lobules, it's considered invasive lobular carcinoma. The lobules are connected to the ducts, which carry breast milk to the nipple.
- Connective tissues. Rarely breast cancer can begin in the connective tissue that's made up of muscles, fat and blood vessels. Cancer that begins in the connective tissue is called sarcoma. Examples of sarcomas that can occur in the breast include phyllodes tumor and angiosarcoma.
How do your cancer cells appear under a microscope?
When a sample of your breast cancer is examined under a microscope, here's what the pathologist looks for:
- Cancer cells with unique appearances. Some subtypes of breast cancer are named for the way they appear under the microscope. Subtypes include tubular, mucinous, medullary and papillary. Your subtype gives your doctor some clues about your prognosis and how your cells may respond to treatment.
- The degree of difference between the cancer cells and normal cells. How different your cancer cells look from normal cells is called your cancer's grade. Breast cancers are graded on a 1 to 3 scale, with grade 3 cancers being the most different looking and considered the most aggressive.
Are your cancer cells fueled by hormones?
Some breast cancers are sensitive to your body's naturally occurring female hormones — estrogen and progesterone. The breast cancer cells have receptors on the outside of their walls that can catch specific hormones that circulate through your body.
Knowing your breast cancer is sensitive to hormones gives your doctor a better idea of how best to treat the cancer or prevent cancer from recurring.
Hormone status of breast cancers includes:
- Estrogen receptor (ER) positive. The cells of this type of breast cancer have receptors that allow them to use the hormone estrogen to grow. Treatment with anti-estrogen hormone (endocrine) therapy can block the growth of the cancer cells.
- Progesterone receptor (PR) positive. This type of breast cancer is sensitive to progesterone, and the cells have receptors that allow them to use this hormone to grow. Treatment with endocrine therapy blocks the growth of the cancer cells.
- Hormone receptor (HR) negative. This type of cancer doesn't have hormone receptors, so it won't be affected by endocrine treatments aimed at blocking hormones in the body.
What is the genetic makeup of your breast cancer cells?
Doctors are just beginning to understand how the individual DNA changes within cancer cells might one day be used to determine treatment options. By analyzing the genes of cancer cells, doctors hope to find ways to target specific aspects of the cancer cells to kill them.
A sample of your tumor tissue from a biopsy procedure may be tested in a laboratory to look for:
- HER2 gene. Cancer cells that have too many copies of the HER2 gene (HER2-positive cancers) produce too much of the growth-promoting protein called HER2. Targeted therapy drugs are available to shut down the HER2 protein, thus slowing the growth and killing these cancer cells.
-
Other tumor markers. Researchers are studying ways to interpret the genetic makeup of tumor cells. Doctors hope this information can be used to predict which cancers will spread and which may need aggressive treatments. That way, women with relatively low-risk breast cancers may avoid aggressive treatments.
Tests that analyze the genetic makeup of breast cancers are available but aren't recommended in all situations. Ask your doctor whether this type of test might be helpful in your case.
Doctors are increasingly using genetic information about breast cancer cells to categorize breast cancers. These groups help guide decisions about which treatments are best. Breast cancer groups include:
- Group 1 (luminal A). This group includes tumors that are ER positive and PR positive, but negative for HER2. Luminal A breast cancers are likely to benefit from hormone therapy and may also benefit from chemotherapy.
- Group 2 (luminal B). This type includes tumors that are ER positive, PR negative and HER2 positive. Luminal B breast cancers are likely to benefit from chemotherapy and may benefit from hormone therapy and treatment targeted to HER2.
- Group 3 (HER2 positive). This type includes tumors that are ER negative and PR negative, but HER2 positive. HER2 breast cancers are likely to benefit from chemotherapy and treatment targeted to HER2.
- Group 4 (basal-like). This type, which is also called triple-negative breast cancer, includes tumors that are ER negative, PR negative and HER2 negative. Basal-like breast cancers are likely to benefit from chemotherapy.
Understanding more about the chemical and genetic makeup of your cancer may help doctors choose the most effective treatment for your specific cancer.
Dec. 06, 2022
- Bleiweiss IJ. Pathology of breast cancer. https://www.uptodate.com/contents/search. Accessed Feb. 7, 2018.
- Niederhuber JE, et al., eds. Cancer of the breast. In: Abeloff's Clinical Oncology. 5th ed. Philadelphia, Pa.: Churchill Livingstone Elsevier; 2014. https://www.clinicalkey.com. Accessed Feb. 7, 2018.
- Breast cancer. Fort Washington, Pa.: National Comprehensive Cancer Network. http://www.nccn.org/professionals/physician_gls/f_guidelines.asp. Accessed Feb. 7, 2018.
- The Cancer Genome Atlas Network. Comprehensive molecular portraits of human breast tumours. Nature. 2012;490:61.