Overview
Wisdom tooth extraction, also called removal, is a surgical procedure to take out one or more wisdom teeth. These are the four permanent adult teeth located at the back corners of your mouth on the top and bottom.
If a wisdom tooth, also known as a third molar, doesn't have room to grow, it can become impacted. If an impacted wisdom tooth causes pain, infection or other dental problems, you'll likely need to have a dentist or an oral surgeon remove it. Some dentists and oral surgeons recommend removing your wisdom teeth, even if they aren't causing problems. That's because these teeth can lead to problems later in life.
Products & Services
Why it's done
Impacted wisdom teeth
Impacted wisdom teeth
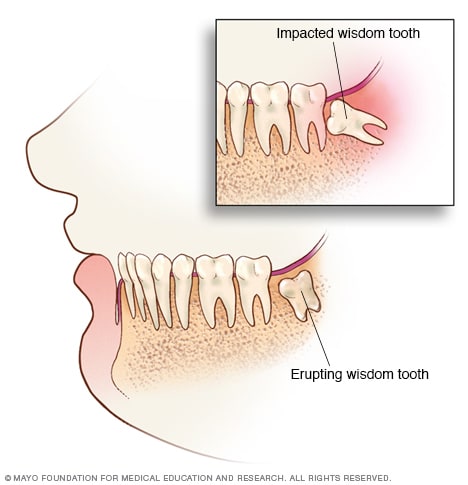
Wisdom teeth are the last of your teeth to appear (erupt) in the mouth. Sometimes a wisdom tooth becomes stuck below the surface of your gums and grows at an odd angle, possibly causing problems. This is called an impacted wisdom tooth.
Wisdom teeth are the last permanent teeth to appear or erupt in the mouth. These teeth usually come through the gums between the ages of 17 and 25. They may come through partially or not at all. Some people's wisdom teeth never come through. For others, wisdom teeth appear just as their other molars did, causing no problems.
Many people have impacted wisdom teeth. These teeth don't have enough room to appear in the mouth as usual.
An impacted wisdom tooth may:
- Grow at an angle toward the next tooth, the second molar.
- Grow at an angle toward the back of the mouth.
- Grow at a right angle to the other teeth, as if the wisdom tooth is "lying down" within the jawbone.
- Grow straight up or down like other teeth but stay trapped within the jawbone.
Problems with impacted wisdom teeth
You'll likely need your impacted wisdom tooth removed if it causes problems such as:
- Pain.
- Trapping food and debris behind the wisdom tooth.
- Infection or gum disease, also known as periodontal disease.
- Tooth decay in a wisdom tooth that partially comes through the gums.
- Damage to a nearby tooth or surrounding bone.
- Development of a fluid-filled sac around the wisdom tooth. This sac also is known as a cyst.
- Complications with braces to straighten other teeth.
Preventing future dental problems
Dental specialists disagree about whether to remove impacted wisdom teeth that aren't causing problems, also known as asymptomatic wisdom teeth. Many dental specialists recommend taking out wisdom teeth that aren't causing any problems. They recommend doing so in the late teens or early 20s. That's because the risk of complications is low, and the procedure usually is safer and patients tolerate it well at this age.
While it's hard to know whether wisdom teeth will become impacted, it may make sense to remove them. That's because:
- Wisdom teeth that aren't causing any problems still could carry disease that can affect you later in life.
- If there isn't enough space for the tooth to come through, it's often hard to clean it properly.
- Serious complications with wisdom teeth happen less often in younger adults.
- Older adults may have a hard time with surgery and have a risk of more complications after surgery to remove them.
Risks
In most cases, the removal of wisdom teeth doesn't cause long-term complications. But you may need surgery to remove impacted wisdom teeth. Often, this surgery is performed with anesthesia to make you sleep and make you more comfortable during the procedure. This surgery involves cutting the gum tissue and taking out some bone around the teeth to remove them safely.
Rarely, surgical complications can include:
- Painful dry socket, or exposure of bone when the blood clot after surgery is lost from the site of the surgical wound. This site also is known as the extraction socket. Your body will heal a dry socket on its own. During this time, you will take medicines to reduce pain.
- Infection in the extraction socket from bacteria or trapped food particles. This usually occurs around two weeks after the procedure.
- Damage to nearby teeth, nerves, jawbone or sinuses.
- Nerve and blood vessel damage.
How you prepare
Your dentist may do the procedure in the office. But if your tooth is deeply impacted or if removing it is tougher than usual, your dentist may suggest that you see an oral surgeon. In addition to numbing the area of your impacted tooth, your surgeon may suggest medicines to help you feel calm or less anxious during the procedure. Or your surgeon will provide you with sedation medicines. These medicines help you sleep through the procedure. They are different from medicines used for general anesthesia, where you are asleep and need to be put on a ventilator to breathe for you. Most wisdom tooth removal procedures occur with sedation where you feel sleepy, but you breathe on your own.
Questions to ask
Questions you may want to ask your dentist or oral surgeon include:
- How many wisdom teeth do you need to remove?
- What type of anesthesia will you use?
- Will this be a difficult procedure?
- How long will the procedure last?
- Have the impacted wisdom teeth damaged other teeth?
- Could this cause nerve damage?
- What other dental treatments will I need?
- How long does it take to heal?
Preparing for surgery
In nearly all cases, wisdom tooth removal is done as an outpatient procedure. This means that you go home the same day.
Staff at the hospital or dental clinic will give you instructions on what to do before the surgery and the day of your scheduled surgery. Ask these questions:
- When should I stop eating food or drinking fluids or both?
- Can I take my prescription medicines before surgery? If so, how soon before surgery can I take them?
- Can I take medicines available without a prescription before surgery?
- When should I arrive at the dental clinic or hospital?
- Will someone need to drive me home after the procedure?
What you can expect
During the procedure
Your dentist or oral surgeon may use one of three types of anesthesia:
- Local anesthesia. Your dentist or oral surgeon gives local anesthesia with one or more shots near where the wisdom tooth is being removed. Before you get a shot, your dentist or surgeon likely will apply a medicine to your gums that will make the injection more comfortable. You're awake during the tooth removal. You'll feel some pressure and movement, but you shouldn't feel pain.
- Sedation anesthesia. Your dentist or oral surgeon gives you medicine through an IV line in your arm to help you feel calm, less anxious and sleepy. You won't feel any pain and won't remember much about the procedure. You'll also get medicine to numb your gums after you become relaxed and feel sleepy.
- General anesthesia. If a procedure is considered complex, you may be given general anesthesia. You may breathe in medicine through your nose or have an IV line in your arm, or both. Then you fall asleep. Once you are asleep, the surgical team will place a breathing tube connected to a ventilator. This machine will breathe for you. While your wisdom teeth are being surgically removed, a doctor called an anesthesiologist, or a certified registered nurse anesthetist, watches your medicine, breathing, temperature, fluids and blood pressure. You'll feel no pain and won't remember the procedure. Medicine also is given to help with pain after the surgery.
Which type of anesthesia you get depends on how hard removing the wisdom is expected to be and your comfort level.
When removing your wisdom tooth, your dentist or oral surgeon:
- Cuts the gum tissue to expose the tooth and bone.
- Removes bone that blocks access to the tooth root.
- Divides the tooth into sections if it's easier to remove in pieces.
- Removes the tooth.
- Cleans the site of the removed tooth of any debris from the tooth or bone.
- Stitches the wound closed to make it heal better, though this isn't always needed.
- Places gauze over the site where the wisdom tooth was removed to control bleeding and help a blood clot form.
After the procedure
If you get sedation anesthesia or general anesthesia, you're taken to a recovery room after the procedure. If you have local anesthesia, you'll likely recover in the dental chair.
As you heal from your surgery, follow your dentist's instructions on:
- Bleeding. Some blood may ooze the first day after a wisdom tooth is removed. Try not to spit too much so that you don't remove the blood clot from the socket. Replace gauze over the surgical site as directed by your dentist or oral surgeon.
- Pain management. You may be able to manage pain with a pain reliever available without a prescription, such as ibuprofen (Advil, Motrin IB, others) or acetaminophen (Tylenol, others), or a mix of both. Or you may take a medicine that your dentist or oral surgeon prescribes. Prescription pain medicine may help if bone was removed during the procedure. Holding an ice pack against your jaw also may ease pain.
- Swelling and bruising. Use an ice pack as directed by your dentist or surgeon. Any swelling of your cheeks usually gets better in two or three days. Bruising may take several more days to get better.
- Activity. After your surgery, plan to relax for the rest of the day. Go back to your usual activities the next day. But for at least a week, don't take part in activities that require a lot of energy that might remove the blood clot from the socket.
- Beverages. Drink a lot of water after the surgery. Don't drink alcoholic, caffeinated, carbonated or hot beverages in the first 24 hours. Don't drink with a straw for at least a week because the sucking action can pull the blood clot from the socket.
- Food. Eat only soft foods, such as yogurt or applesauce, for the first 24 hours. Start eating foods that are somewhat soft when you can tolerate them. Do not eat hard, chewy, hot or spicy foods that might get stuck in the socket or irritate the wound.
- Cleaning your mouth. Don't brush your teeth, rinse your mouth, spit or use mouthwash during the first 24 hours after surgery. Usually, you'll be told to go back to brushing your teeth after the first 24 hours. Be gentle near the surgical wound when brushing. Gently rinse your mouth with warm saltwater every two hours and after meals for a week.
- Tobacco use. If you smoke, don't do so for at least 72 hours after surgery. Wait longer if possible. If you chew tobacco, don't use it for at least a week. Using tobacco products after oral surgery can delay healing and raise the risk of complications.
- Stitches. You may have stitches that dissolve within a few weeks. Or you may not have any stitches. If your stitches need to be removed, schedule an appointment to have them taken out.
When to call your dentist or surgeon
Call your dentist or oral surgeon if you have any of these symptoms:
- A hard time swallowing or breathing.
- Too much bleeding.
- Fever.
- Severe pain not relieved by prescribed pain medicines.
- Swelling that worsens after two or three days.
- A bad taste in your mouth that saltwater rinsing does not remove.
- Pus in the socket or blood or another fluid that slowly leaks out of the socket.
- Lasting numbness or loss of feeling.
- Blood or pus in nasal discharge.
These symptoms could mean that you have an infection, nerve damage or other serious complications.
Results
You probably won't need a follow-up appointment after a wisdom tooth is removed if:
- You have no stitches to remove.
- No complications arose during the procedure.
- You don't have lasting problems, such as pain, swelling, numbness or bleeding — complications that might mean you have an infection, nerve damage or other problems.
If you have complications, contact your dentist or oral surgeon to talk about treatment options.