Overview
Whipple procedure
Whipple procedure
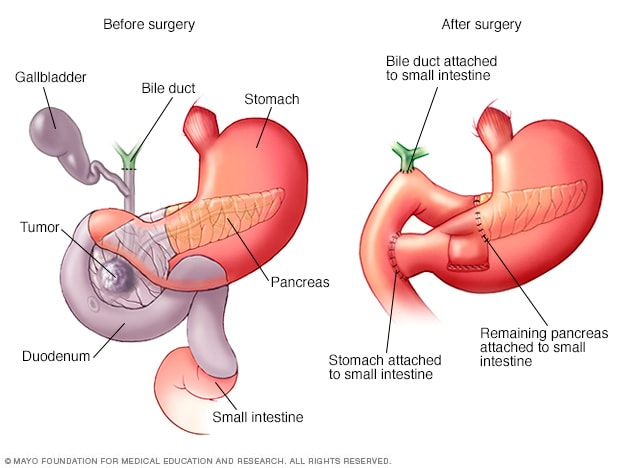
The Whipple procedure, also called pancreaticoduodenectomy, is an operation to remove the head of the pancreas. The operation also involves removing the first part of the small intestine, called the duodenum, the gallbladder and the bile duct. The remaining organs are rejoined to allow food to move through the digestive system after surgery.
The Whipple procedure is an operation to treat tumors and other conditions in the pancreas, small intestine and bile ducts. It involves removing the head of the pancreas, the first part of the small intestine, the gallbladder and the bile duct.
The Whipple procedure is also called a pancreaticoduodenectomy. It's often used to treat pancreatic cancer that hasn't spread beyond the pancreas.
The Whipple procedure is a complex operation. It can have serious risks. However, this surgery often saves lives.
Related procedures
There are other types of pancreas operations. Your surgeon may talk with you about these other procedures in certain situations. Seek a second opinion from a specialized surgeon if needed. Related procedures include:
- Surgery for tumors or other conditions in the body and tail of the pancreas. The body and tail of the pancreas make up the left side of the organ. Surgery to remove the left side of the pancreas is called a distal pancreatectomy. During this procedure, the surgeon also might need to remove the spleen.
- Surgery to remove the whole pancreas. This is called total pancreatectomy. After the pancreas is removed, you'll take medicine to replace the hormones and enzymes made by the pancreas for the rest of your life.
- Surgery for tumors that affect nearby blood vessels. When a tumor in the pancreas grows to involve nearby blood vessels, a more-complex procedure might be needed. The procedure might need to involve taking out and rebuilding parts of the blood vessels. Few medical centers in the United States have surgeons trained to do these blood vessel operations safely.
Why it's done
The Whipple procedure might be a treatment option for cancers or other conditions in the pancreas, bile duct, or the first part of the small intestine, called the duodenum.
The pancreas is a vital organ that lies in the upper belly, behind the stomach. It works closely with the liver and the ducts that carry bile.
The pancreas releases proteins called enzymes that help digest food. The pancreas also makes hormones that help manage blood sugar.
A Whipple procedure might treat:
- Pancreatic cancer.
- Pancreatic cysts.
- Pancreatic tumors.
- Pancreatitis.
- Ampullary cancer.
- Bile duct cancer, also called cholangiocarcinoma.
- Neuroendocrine tumors.
- Small intestine cancer, also called small bowel cancer.
- Trauma to the pancreas or small intestine.
- Other tumors or conditions in the pancreas, duodenum or bile ducts.
The goal of doing a Whipple procedure for cancer is to remove the cancer and prevent it from growing and spreading to other organs. For many of these cancers, the Whipple procedure is the only treatment that can lead to long-term survival and cure.
Risks
The Whipple procedure is a difficult operation. It has risks both during and after surgery, including:
- Bleeding.
- Infection, which can happen inside the belly or on the skin that was cut during surgery.
- Slow emptying of the stomach, which may make it hard for a time to eat or to keep food down.
- A leakage from where the pancreas or bile duct connect.
- Diabetes, which can be short-lived or lifelong.
Research shows that it's best to have this surgery at a medical center where surgeons have done many of these operations. These centers tend to have better results and fewer complications. Be sure to ask how many Whipple procedures and other pancreatic operations your surgeon and the hospital have done. If you have doubts, get a second opinion.
How you prepare
Before the Whipple procedure, you meet with your surgeon and health care team to discuss what to expect before, during and after surgery, and the possible risks. Your care team talks with you and your family about how the surgery will affect your life. This is a good time to talk with your care team about any worries you might have.
Sometimes, you may get treatment such as chemotherapy, radiation therapy or both before a Whipple procedure or other pancreas operation. Ask your health care team about whether you need these other treatment options before or after the operation.
What to expect with your operation may depend on the type of procedure you have. There are different ways to do the Whipple procedure. To make sure you get the surgery that's best for you, your surgeon considers your condition and general health. You need to be healthy enough for a difficult operation. You might need more medical tests before surgery.
The Whipple procedure might be done as:
- Open surgery. During an open operation, a surgeon makes a cut, called an incision, through the belly to get to the pancreas. This is the most common approach.
- Laparoscopic surgery. This surgery also is called minimally invasive surgery. The surgeon makes several smaller cuts in the belly and puts special tools through them. The tools include a camera that sends video to a monitor in the operating room. The surgeon watches the monitor to guide the surgical tools in doing the Whipple procedure.
- Robotic surgery. Robotic surgery is another type of minimally invasive surgery. The surgical tools are attached to a mechanical device called a robot. The surgeon sits at a console nearby and uses hand controls to direct the robot. A surgical robot can use tools in tight spaces and around corners, where human hands might be too large to work well.
Minimally invasive surgery has some benefits. They include less blood loss and a faster recovery when there are no complications.
Sometimes when a procedure begins as minimally invasive surgery, complications or other issues require the surgeon to switch to open surgery to finish the operation.
Before going to the hospital for surgery, tell family or friends about help you'll need from them when you get home. You will likely need help for the first couple of weeks after leaving the hospital. Talk to your care team about what you need to do during your recovery at home.

A Mayo Clinic surgeon talks with a patient about the Whipple procedure.
What you can expect
Before the procedure
The morning of surgery, you check into the hospital and register. Nurses and other staff members make sure of your name, date of birth, procedure and surgeon. You then change into a surgical gown to get ready for surgery.
Before your surgery, an intravenous line, also called an IV, is put into a vein. The IV usually goes into your arm. The IV lets your care team put fluid and medicines into your body as needed. You also may get medicine to help you relax if you're nervous.
You might have procedures that will help reduce pain after surgery. For example, you might have a thin tube placed into the space near your spine, called the epidural space. The tube can deliver medicine to control pain. Or you might have shots of medicine in the spine or abdomen. These procedures can help lower pain levels after surgery. They can lower the need for strong pain medicines as you recover.
During the procedure
The surgical team includes pancreatic surgeons and surgical nurses. The team also includes doctors and nurses trained in giving the medicine that puts you in a sleep-like state during surgery, called anesthesiologists and anesthetists. The Whipple procedure is done using general anesthesia. This means you'll be in a sleep-like state during the entire operation.
After the anesthesia takes effect, a tube is put into your bladder. The tube is called a urinary catheter. It drains urine during and after surgery. The catheter is usually removed one or two days after surgery.
Surgery may take 4 to 12 hours. The time depends on the approach to surgery and how difficult the operation is.
During a Whipple procedure, the surgeon removes:
- The head of the pancreas.
- The first part of the small intestine, called the duodenum.
- The gallbladder.
- The bile duct.
Sometimes, the Whipple procedure also involves taking out part of the stomach or the nearby lymph nodes.
At the end of the Whipple procedure, the surgeon rejoins the remaining organs to allow food to move through the digestive system.
After the procedure
After your Whipple procedure, you can expect to spend at least a week in the hospital. How long you need to stay in the hospital depends on how your recovery goes.
After your surgery, you'll be moved to a hospital room to begin recovery. Most people go to a general surgical nursing floor in the hospital. Nursing staff and the surgical team check on you several times a day to watch for signs of infection or other complications.
As your digestive system recovers after surgery, you'll likely start by drinking clear liquids. Foods may be added to your diet slowly. Most people are able to get up and walk soon after the operation.
Some people may need to spend a few days in the intensive care unit, also called the ICU, right after surgery. In the ICU, doctors and nurses monitor you closely to watch for signs of complications. You might need to spend time in the ICU if you have certain medical conditions.
After leaving the hospital, most people can go home to recover. Some people might stay nearby for several days to be watched and have follow-up visits. Older adults and people with other health concerns might go to a skilled rehabilitation facility. This is a place that can help you rebuild strength until you're ready to return home. Talk to your health care team if you're worried about going home.
Most people return to their usual activities 4 to 6 weeks after surgery. How long it takes you to recover depends on your health before your surgery and how difficult your surgery was.
Results
The chances of long-term survival after a Whipple procedure depend on many factors. Talk with your health care team about what you can expect. For most tumors and cancers in the pancreas, the Whipple procedure is the only known cure.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.