Overview
Left ventricular assist device (LVAD)
Left ventricular assist device (LVAD)
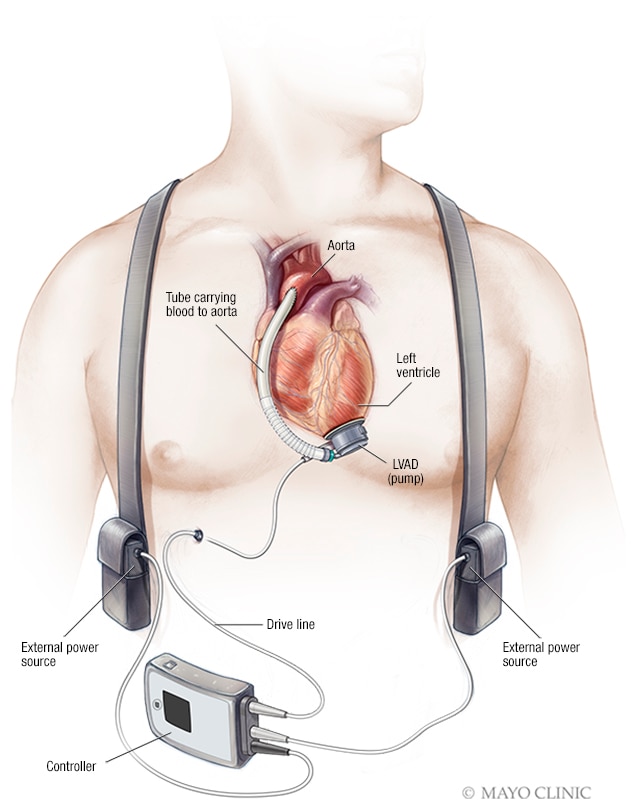
A left ventricular assist device (LVAD) is implanted in the chest. It helps pump blood from the lower left heart chamber, called the left ventricle, to the rest of the body. A controller unit and battery pack are worn outside the body and are connected to the LVAD through a small opening in the skin.
A ventricular assist device (VAD) is a device that helps pump blood from the lower chambers of the heart to the rest of the body. It's a treatment for a weakened heart or heart failure. A VAD may be used to help the heart work while waiting for other treatments, such as a heart transplant. Sometimes a VAD is used to permanently help the heart pump blood.
Another name for a VAD is a durable mechanical circulatory support device.
A VAD is most frequently placed in the left lower heart chamber, called the left ventricle. When placed in the left ventricle, it's called a left ventricular assist device (LVAD). This article focuses on LVADs.
Current LVADs provide a constant flow of blood from the heart to the body. They also are called continuous flow devices.
Getting an LVAD often requires open-heart surgery and has serious risks. However, an LVAD can be lifesaving if you have severe heart failure.
Ventricular assist device (VAD) Overview
Products & Services
Why it's done
Your health care provider may recommend a left ventricular assist device (LVAD) if:
- You're waiting for a heart transplant. An LVAD may be temporarily used while you wait for a donor heart to become available. This type of treatment is called a bridge to transplant. An LVAD can keep blood pumping through your body despite a damaged heart. It will be removed when you receive your new heart. An LVAD also may help other organs in the body work better while you're waiting for a heart transplant. LVADs can sometimes lower pressures in the lungs. High lung pressures can prevent someone from being able to receive a heart transplant.
- You can't have a heart transplant because of age or other factors. Sometimes it's not possible to have a heart transplant. So an LVAD may be used as a permanent treatment. This use of a ventricular assist device is called destination therapy. If you have heart failure, it may improve your quality of life.
- You have temporary heart failure. If your heart failure is temporary, your heart doctor may recommend having an LVAD until your heart can pump blood on its own again. This type of treatment is called a bridge to recovery.
To decide if an LVAD is the right treatment for your condition, and to select which device is best for you, your heart doctor considers:
- The severity of your heart failure.
- Other serious medical conditions you have.
- How well the main pumping chambers of the heart are working.
- Your ability to safely take blood thinners.
- How much social support you have from your family and friends.
- Your mental health and ability to take care of a VAD.
Risks
Possible risks and complications of a ventricular assist device (VAD) include:
- Bleeding. Any surgery can increase your risk of bleeding.
- Blood clots. As blood moves through the device, blood clots may form. A blood clot can slow or block blood flow. This can cause problems with the device or a stroke.
- Infection. The power source and controller for an LVAD are located outside the body and are connected through a wire through a small opening in your skin. Germs could infect this area. This can cause an infection at the site or in your blood.
- Device problems. Sometimes an LVAD may stop working correctly after it's implanted. For example, if there is damage to the wires, the device may not pump blood properly. This problem needs immediate medical attention. The pump may need to be replaced.
- Right heart failure. If you have an LVAD, the lower left chamber of the heart will pump more blood than it used to. The lower right chamber may be too weak to manage the increased amount of blood. Sometimes this requires a temporary pump. Medicines or other therapies may help the lower right chamber pump better in the long term.
How you prepare
If you're getting an LVAD, you'll need surgery to implant the device. Before surgery, your health care team will:
- Tell you what to expect before, during and after the surgery.
- Explain the possible risks of VAD surgery.
- Discuss any concerns you have.
- Ask if you have an advance directive.
- Give you specific instructions to follow during your recovery at home.
You can prepare for LVAD surgery by talking to your family about your upcoming hospital stay. Also talk about the type of help you'll need at home as you recover.
Food and medications
Bring a list of all the medicines you take with you to the hospital. Also note if you have any allergies to medicines. Your health care team reviews your medicines before surgery.
You'll likely need to stop eating or drinking for several hours before surgery. Your health care team gives you specific instructions.
Clothing and personal items
Bring these items with you to the hospital:
- A copy of your advance directive, if you have one.
- Eyeglasses, hearing aids or dentures.
- Personal care items, such as a toothbrush, a hairbrush or comb, and shaving equipment.
- Loosefitting, comfortable clothing.
- Items that may help you relax, such as portable music players or books.
You'll likely be asked to avoid wearing:
- Contact lenses.
- Dentures.
- Eyeglasses.
- Jewelry.
- Nail polish.
What you can expect
Before the procedure
You may be admitted to the hospital a few days before getting an LVAD. While you're in the hospital, you may have other treatments for your weakened heart or heart failure.
During this time, tests are done to make sure an LVAD is still your best treatment option. Tests may include:
- Blood tests. Different blood tests are done to see how well the heart, liver, kidneys and other organs are working. A complete blood count and blood clotting studies are done to make sure your blood isn't too thin for surgery.
- Electrocardiogram (ECG or EKG). This quick and painless test records the electrical signals in the heart. It can show the rhythm of the heart and how fast or how slowly the heart is beating.
- Chest X-ray. A chest X-ray shows the size and shape of the heart and can show certain problems with the lungs.
- Echocardiogram. Sound waves create images of the heart in motion. This test shows the structure of the heart and heart valves and blood flow through the heart. An echocardiogram can help determine whether a ventricular assist device is the right treatment option.
- Cardiac catheterization. A long, thin flexible tube called a catheter is inserted in a blood vessel, usually in the neck. It's moved to the heart using X-rays as a guide. During this test, pressures and blood flow in the heart can be checked. This test can help determine if an LVAD or other treatment is needed.
During the procedure
Getting an LVAD often requires open-heart surgery. The surgery usually takes three or more hours. You can expect the following:
- Any hair on the chest is shaved from the area where surgery will take place.
- You'll get medicines through an IV to make you sleepy and pain-free during the surgery.
- You'll be connected to a machine that helps you breathe during your surgery. This machine is called a ventilator.
- Your heart may be stopped using medicines during the surgery. If so, you'll be connected to a heart-lung bypass machine. The machine keeps oxygen-rich blood flowing through your body during surgery.
If you're getting a left ventricular assist device (LVAD), the surgeon makes a cut down the center of the chest. The surgeon separates the chest bone to better view the heart and then places the device.
An LVAD has several parts.
- The main pump is inserted into the tip of the heart.
- The blood pumps through a flexible plastic tube to the body's main artery, called the aorta.
- The aorta sends blood to the rest of the body.
- A cord inserted through an opening in the skin connects the pump to a control unit and battery pack outside the body.
After your LVAD is in place and working properly, you'll be taken off the heart-lung bypass machine so your LVAD can start pumping blood.
After the procedure
You stay in the hospital after LVAD surgery. How long you stay in the hospital depends on your health before the surgery and how quickly you recover.
At the hospital, your health care team watches you for complications. Tubes drain urine from your bladder. Tubes also drain fluid and blood from your heart and chest.
You usually receive:
- Fluids and medicines given by IV.
- Antibiotics to prevent infections.
- Blood-thinning medicine to prevent blood clots.
You may be on a breathing machine, called a ventilator, for a few days.
As you recover in the hospital, your health care team helps you become more active and stronger. They'll help you sit up, get out of bed and walk. If you need more time to improve your strength, a short stay at a rehabilitation center may be recommended.
Before you leave the hospital, your health care team talks to you and your family about how to live with and properly care for an LVAD. Some of the things you'll learn include:
- How to clean the skin where the LVAD was placed.
- What to do if there are symptoms of infection, including fever and pain, redness, or drainage.
- How to keep the device charged. It's important to always have spare batteries with you.
- How to check the controller for dirt and the batteries for damage.
- What to do if the LVAD isn't working properly.
- How to shower without damaging the device.
- What to do if the device's alarm goes off.
Your health care team tells you when you can safely return to daily life activities such as driving, exercising, going to work or being sexually active. You'll also get tips on how to safely travel with an LVAD.
Don't hesitate to talk to your health care team if you have any concerns about living with a ventricular assist device.
Results
After getting an LVAD, you have regular checkups to watch for complications and improve your health. A member of your health care team makes sure the LVAD is working as it should. You may have special tests to check your blood pressure.
You'll be prescribed a blood-thinning medicine to help prevent blood clots. You'll need regular blood tests to check the medicine's effects.
Cardiac rehabilitation
After getting an LVAD, your health care provider may recommend a personalized exercise and education program. The program is called cardiac rehabilitation. It teaches you ways to improve your heart health after heart surgery. The program often includes supervised exercise, heart-healthy diet tips and emotional support.
LVADs and heart transplants
If you have an LVAD to help your heart pump blood while you wait for a heart transplant, you'll remain in close contact with your health care team while you're on the waiting list. You'll likely be told not to travel far so you're close to the hospital in case a donor heart becomes available.
Coping and support
If you're feeling anxious or frustrated about living with an LVAD, consider talking to your health care provider or a counselor. Connecting with others in a support group may help lower stress and anxiety. A support group lets you share your thoughts and feelings with others who have similar experiences.