Overview
Parts of the immune system
Parts of the immune system
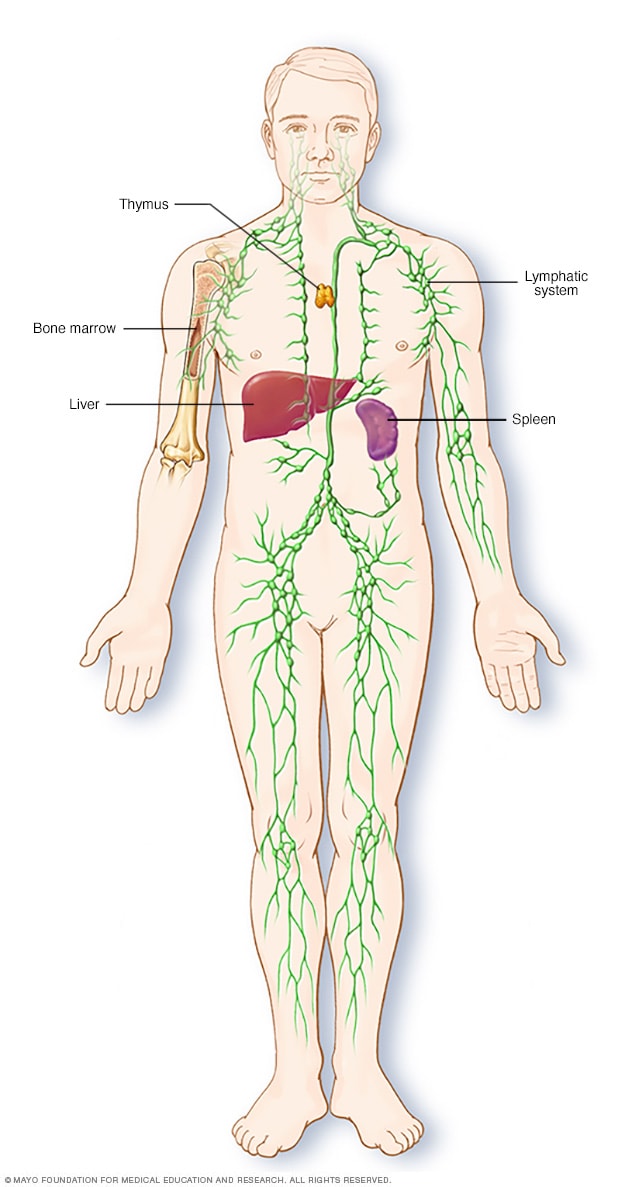
The lymphatic system is part of the body's immune system, which protects against infection and disease. The lymphatic system includes the spleen, thymus, lymph nodes and lymph channels, as well as the tonsils and adenoids.
Splenectomy is a surgical procedure to remove your spleen. The spleen is an organ that sits under your rib cage on the upper left side of your abdomen. It helps fight infection and filters unneeded material, such as old or damaged blood cells, from your blood.
The most common reason for splenectomy is to treat a ruptured spleen, which is often caused by an abdominal injury. Splenectomy may be used to treat other conditions, including an enlarged spleen that is causing discomfort (splenomegaly), some blood disorders, certain cancers, infection, and noncancerous cysts or tumors.
Splenectomy is most commonly performed using a tiny video camera and special surgical tools (laparoscopic splenectomy). With this type of surgery, you may be able to leave the hospital the same day and recover fully in two weeks.
Why it's done
Splenectomy is used to treat a wide variety of diseases and conditions. Your doctor may recommend splenectomy if you have one of the following:
- Ruptured spleen. If your spleen ruptures due to a severe abdominal injury or because of an enlarged spleen (splenomegaly), the result may be life-threatening, internal bleeding.
- Enlarged spleen. Splenectomy may be done to ease the symptoms of an enlarged spleen, which include pain and a feeling of fullness.
- Blood disorder. Blood disorders that may be treated with splenectomy include idiopathic thrombocytopenic purpura, polycythemia vera and thalassemia. But splenectomy is typically performed only after other treatments have failed to reduce the symptoms of these disorders.
- Cancer. Cancers that may be treated with splenectomy include chronic lymphocytic leukemia, Hodgkin's lymphoma, non-Hodgkin's lymphoma and hairy cell leukemia.
- Infection. A severe infection or the development of a large collection of pus surrounded by inflammation (abscess) in your spleen may require spleen removal if it doesn't respond to other treatment.
- Cyst or tumor. Noncancerous cysts or tumors inside the spleen may require splenectomy if they become large or are difficult to remove completely.
Your doctor may also remove your spleen to help diagnose a condition, especially if you have an enlarged spleen and he or she can't determine why.
Risks
Splenectomy is generally a safe procedure. But as with any surgery, splenectomy carries the potential risk of complications, including:
- Bleeding
- Blood clots
- Infection
- Injury to nearby organs, including your stomach, pancreas and colon
Long-term risk of infection
After spleen removal, you're more likely to contract serious or life-threatening infections. Your doctor may recommend that you receive vaccines against pneumonia, influenza, Haemophilus influenzae type b (Hib) and meningococci. He or she may also recommend that you take preventive antibiotics, especially if you have other conditions that increase your risk of serious infections.
How you prepare
Food and medications
Before your procedure, you may need to temporarily stop taking certain medications and supplements. You may also need to avoid eating or drinking for a certain amount of time. Your doctor will give you specific instructions to help you prepare.
Other precautions
If you have time before the surgery, you may need to receive blood transfusions to ensure that you have enough blood cells after your spleen is removed.
Your doctor may also recommend that you receive a pneumococcal vaccine and possibly other vaccines to help prevent infection after your spleen is removed.
What you can expect
Before the procedure
Right before your surgery, you will be given a general anesthetic. The anesthesiologist or anesthetist gives you an anesthetic medication such as a gas — to breathe through a mask — or as a liquid injected into a vein. The surgical team monitors your heart rate, blood pressure and blood oxygen throughout the procedure. You will have heart monitor leads attached to your chest and a blood pressure cuff on your arm.
During the procedure
After you're unconscious, your surgeon begins the surgery using either a minimally invasive (laparoscopic) or open (traditional) procedure. The method used often depends on the size of the spleen. The larger the spleen, the more likely your surgeon will choose to do an open splenectomy.
-
Laparoscopic splenectomy. During laparoscopic splenectomy, the surgeon makes four small incisions in your abdomen. He or she then inserts a tube with a tiny video camera into your abdomen through one of the incisions. Your surgeon watches the video images on a monitor and removes the spleen with special surgical tools that are put in the other three incisions. Then he or she closes the incisions.
Laparoscopic splenectomy isn't appropriate for everyone. A ruptured spleen usually requires open splenectomy. In some cases a surgeon may begin with a laparoscopic approach and find it necessary to make a larger incision because of scar tissue from previous operations or other complications.
- Open splenectomy. During open splenectomy, the surgeon makes an incision in the middle of your abdomen and moves aside muscle and other tissue to reveal your spleen. He or she then removes the spleen and closes the incision.
After the procedure
- In the hospital. After surgery, you're moved to a recovery room. If you had laparoscopic surgery, you'll likely go home the same day or the day after. If you had open surgery, you may be able to go home after two to six days.
- After you go home. Talk to your doctor about how long to wait until resuming your daily activities. If you had laparoscopic surgery, it may be two weeks. After open surgery, it may be six weeks.
Results
If you had splenectomy due to a ruptured spleen, further treatment usually isn't necessary. If it was done to treat another disorder, additional treatment may be required.
Life without a spleen
After splenectomy, other organs in your body take over most of the functions previously performed by your spleen. You can be active without a spleen, but you're at increased risk of becoming sick or getting serious infections. This risk is highest shortly after surgery. People without a spleen may also have a harder time recovering from an illness or injury.
To reduce your risk of infection, your doctor may recommend vaccines against pneumonia, influenza, Haemophilus influenzae type b (Hib) and meningococci. In some cases, he or she may also recommend preventive antibiotics, especially for children under 5 and those with other conditions that increase the risk of serious infections.
After splenectomy, notify your doctor at the first sign of an infection, such as:
- A fever of 100.4 F (38 C) or higher
- Redness or tender spots anywhere on the body
- A sore throat
- Chills that cause you to shake or shiver
- A cold that lasts longer than usual
Make sure anyone caring for you knows that you've had your spleen removed. Consider wearing a medical alert bracelet that indicates that you don't have a spleen.