Overview
Prostatectomy is surgery to remove part or all of the prostate gland. The prostate gland is part of the male reproductive system. It's located in the pelvis, below the bladder. It surrounds the hollow tube called the urethra that carries urine from the bladder to the penis.
Prostatectomy can treat certain conditions that affect the prostate. It's most commonly used as a treatment for prostate cancer.
Prostatectomy can be done in various ways, depending on the condition involved. For instance, sometimes surgery can be done through small cuts, also called incisions. This is known as minimally invasive surgery. If you get this type, your surgeon may even control a robotic device to help operate. Other times, surgery needs to be done through one larger cut. This is called traditional open surgery.
Mayo Clinic urologists use advanced endoscopic techniques to address enlarged prostate symptoms without the need for open, laparoscopic or robotic surgery in most cases.
Products & Services
Why it's done
Most often, prostatectomy is done to treat cancer that likely hasn't spread beyond the prostate gland. The entire prostate and some tissue around it are removed. This surgery is called radical prostatectomy. During surgery, any nearby lymph nodes that look unusual also may be removed and checked for cancer. Radical prostatectomy may be used alone, or along with radiation or hormone therapy.
A surgeon can do a radical prostatectomy using different techniques, including:
- Robot-assisted radical prostatectomy. The surgeon makes 5 to 6 small incisions in the lower stomach area to remove the prostate. The surgeon sits at a computer console and controls surgical tools that are attached to robotic arms. Robot-assisted surgery lets the surgeon operate with precise movements. It may cause less pain than open surgery, and recovery time may be shorter.
- Open radical prostatectomy. The surgeon typically makes an incision in the lower abdomen to remove the prostate.
Prostatectomy can treat health conditions other than cancer. For these conditions, often part of the prostate is removed. This is called a simple prostatectomy. It can be a treatment choice for some people with serious urinary symptoms and very enlarged prostate glands. An enlarged prostate is known as benign prostatic hyperplasia (BPH).
Simple prostatectomy often is done as minimally invasive surgery with robotic assistance. It's not often done as open surgery anymore.
Simple prostatectomy to treat BPH removes just the part of the prostate that's blocking the flow of urine. The surgery eases urinary symptoms and complications resulting from blocked urine flow, including:
- A frequent, urgent need to urinate.
- Trouble starting urination.
- Slow urination, also called prolonged urination.
- Urinating more than usual at night.
- Stopping and starting again while urinating.
- The feeling that you can't fully empty your bladder.
- Urinary tract infections.
- Not being able to urinate.
Mayo Clinic urologists use advanced endoscopic techniques to address these symptoms without incisions in most cases.
Your surgical team talks with you about the pros and cons of each technique. You also talk about your preferences. Together, you and your surgical team decide which approach is best for you.
 Explaining prostatectomy options
Explaining prostatectomy options
A Mayo Clinic urologist explains prostatectomy options.
Risks
Radical prostatectomy risks
Any surgery comes with risks. Risks of radical prostatectomy include:
- Bleeding.
- Urinary tract infection.
- The loss of bladder control, also called urinary incontinence. This often goes away over time.
- Trouble getting and keeping an erection that's firm enough for sex, also called erectile dysfunction.
- Narrowing of the tube through which urine leaves the body, called the urethra. Or narrowing of the neck of the bladder, where the urethra and bladder meet.
- A collection of fluid called lymph.
- Rarely, damage to the intestine or rectum.
At Mayo Clinic, the urologists who do prostatectomies have advanced training and extensive experience in all aspects of the surgery. Much of this expertise stems from the high numbers of people treated: More robotic surgery is done at Mayo Clinic than anywhere else in the world. Plus, Mayo healthcare professionals with various areas of expertise work together to help manage care. This ensures the lowest complication rates and delivers the best outcomes possible for people who have this surgery.
Simple prostatectomy risks
Simple prostatectomy works well at easing urinary symptoms. But it has a higher risk of complications and a longer recovery time than some other enlarged prostate treatments. These treatments include transurethral resection of the prostate (TURP), laser PVP surgery and holmium laser prostate surgery (HoLEP).
Risks of simple prostatectomy include:
- Bleeding.
- Urinary tract infection.
- Urinary incontinence.
- Semen going into the bladder instead of leaving the body through the penis during ejaculation. This is called retrograde ejaculation.
- Erectile dysfunction.
- Narrowing of the urethra or bladder neck after open surgery.
How you prepare
Before surgery, your surgeon may do a test called cystoscopy that uses a device called a scope to look inside your urethra and bladder. Cystoscopy lets your surgeon check the size of your prostate and examine your urinary system. Your surgeon also may want to do other tests. These include blood tests or tests that measure your prostate and measure urine flow.
Follow your surgery team's instructions on what to do before your treatment.
Food and medications
Talk with your surgery care team about:
- Your medicines. Tell your surgery team about any medicines or supplements you take, whether you need prescriptions for them or not. This is extra important if you take blood-thinning medicines such as warfarin or clopidogrel (Plavix). It's also very important to tell your care team if you take pain relievers that are sold without a prescription. These include aspirin, ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve). Your surgeon may ask you to stop taking medicines that raise your risk of bleeding a certain number of days before the surgery.
- Medicine allergies or reactions. Talk to your surgery team about any allergies or reactions you have had to medicines.
- Fasting before surgery. Your surgeon likely will ask that you not eat or drink anything after midnight. On the morning of your surgery, take only the medicines your surgeon tells you to with a small sip of water.
- Bowel prep before surgery. You may be given a kit and instructions to help clear your bowels before surgery. The kit contains items that help you insert water into your rectum to empty your bowels. This is known as giving yourself an enema.
Clothing and personal items
Plan to avoid wearing these items into surgery:
- Jewelry.
- Eyeglasses.
- Contact lenses.
- Dentures.
Arrangements after surgery
Ask your surgeon how long you'll be in the hospital. You'll want to arrange in advance for a ride home. You won't be able to drive yourself right after surgery.
Activity restrictions
You may not be able to work or do strenuous activities for weeks after surgery. Ask your surgeon how much recovery time you may need.
What you can expect
Before the procedure
Most often, prostatectomy is done using medicine to prevent pain and put you in a sleep-like state. This is called general anesthesia. Your surgeon also may give you an antibiotic right before surgery to help prevent infection with germs.
During the procedure
Prostatectomy incisions
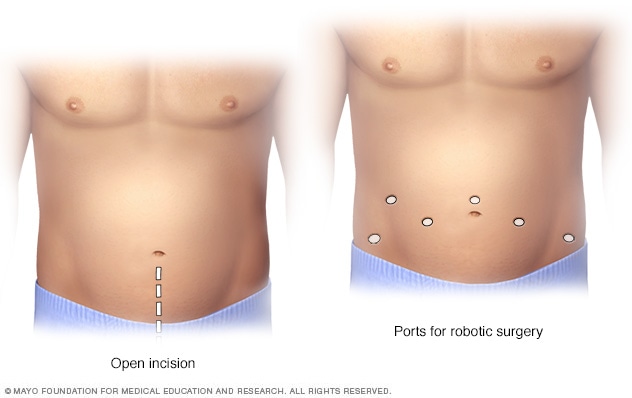
Prostatectomy incisions
During an open prostatectomy, one large incision is made in the lower stomach area (left). During a robotic prostatectomy, several smaller incisions are made in the stomach area (right).
Robot-assisted radical prostatectomy. Your surgeon sits at a remote-control console a short distance from you and the operating table. The surgeon precisely controls the motion of the surgical tools using two hand-and-finger control devices. The console displays a magnified, 3D view of the surgical area. This lets the surgeon picture the surgery in much more detail than in traditional laparoscopic surgery.
The robotic system lets the surgeon make smaller and more-precise incisions. This helps some people recover faster than traditional open surgery does. The robotic approach also can help surgeons save the nerves that are attached to each side of the prostate. This may prevent some younger people from getting erectile dysfunction due to nerve injuries during surgery.
- Open radical prostatectomy. The surgeon makes an incision in the lower stomach area, from below the navel to just above the pubic bone. The prostate gland is carefully separated from surrounding nerves and blood vessels. Then the surgeon removes the prostate along with nearby tissue. The incision is closed with sutures.
Simple prostatectomy. At the start of the surgery, the surgeon may insert a long, flexible viewing scope called a cystoscope through the tip of the penis. This lets the surgeon see inside the urethra, bladder and prostate area. The surgeon then inserts a tube called a catheter into the tip of the penis. The catheter extends into the bladder to drain urine during the surgery. Where the incisions are made depends on the technique your surgeon uses. If you also have a hernia or bladder condition, your surgeon may use the surgery as a chance to repair it.
Once the surgeon has removed the part of the prostate causing symptoms, 1 to 2 drain tubes may be inserted. The tubes are placed through punctures in the skin near the surgery site. One tube goes directly into the bladder. The other tube goes into the area where the prostate was removed. In time, the tubes are removed.
After the procedure
After surgery you should expect that:
- You'll likely be given pain medicines through a vein (IV). Your surgeon may give you prescription pain pills to take after the IV tube is removed.
- Your surgeon likely will have you walk the day of or the day after surgery. You'll also do exercises to move your feet while you're in bed.
- You'll likely go home 1 to 2 days after surgery. When your surgeon thinks it's safe for you to go home, the pelvic drain is taken out. You may need to return to the surgeon in one or two weeks to have staples taken out.
- You'll likely return home with a catheter in place. Most people need a urinary catheter for 7 to 10 days after surgery. Full recovery of urinary control can take up to a year after surgery.
Make sure you understand the self-care measures you need to take after surgery. Also understand any restrictions you need to follow, such as limits on driving or lifting heavy things:
- You'll need to resume your activity level slowly over time. You should be back to your usual routine in about 4 to 6 weeks.
- You'll need to see your healthcare professional a few times to make sure everything is OK. Most people who get prostatectomies see their healthcare professional after about six weeks. Then they get healthcare checkups every three months for the first year, and twice in the second year after surgery. If you have any health issues or concerns, you may need to see your healthcare professional sooner or more often.
- You'll likely be able to resume sexual activity after recovering from surgery. After simple prostatectomy, you can still have an orgasm during sex. But you may ejaculate very little or no semen. Ask your surgeon how long it may take before you can get and keep erections firm enough for sex. Some older people may not regain sexual function after surgery.
Results
Compared with an open prostatectomy, robot-assisted prostatectomy can result in:
- Less pain and blood loss.
- Less tissue trauma.
- A shorter hospital stay.
- A quicker recovery.
You typically can return to your usual activities with minor limits around four weeks after surgery.
Simple prostatectomy provides long-term relief of urinary symptoms due to an enlarged prostate. It's the most invasive procedure to treat an enlarged prostate, but serious complications are rare. Most people who have the surgery don't need any follow-up treatment for their BPH.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Sept. 07, 2024