Risks
Risks of a mastectomy include:
- Bleeding.
- Infection.
- Delayed healing.
- Pain.
- Swelling in your arm if you have an axillary node dissection, called lymphedema.
- Formation of hard scar tissue at the surgical site.
- Shoulder pain and stiffness.
- Numbness in the chest.
- Numbness under your arm from lymph node removal.
- Buildup of blood in the surgical site, called hematoma.
- Changes in the way your chest or breasts look after surgery.
- Changes in the way you feel about your body after surgery.
How you prepare
Meet with your surgeon to discuss your options
Before your surgery, you'll meet with members of your surgical team to discuss your operation. This is a good time to ask questions and to make sure you understand the procedure, including the reasons for surgery, the risks and other treatment options.
Your surgeon may talk about breast reconstruction with you. Breast reconstruction is surgery to restore shape to the breast. Many factors go into deciding whether reconstruction can be done and when. Sometimes it's possible to have the reconstruction done right away after your mastectomy. Typically, the reconstruction is started at the time of your mastectomy and is completed with another procedure several months later. Sometimes, reconstruction may involve more than one procedure.
Breast reconstruction may involve using:
- Breast expanders with saline or silicone implants.
- Your body's own tissue, called autologous tissue reconstruction.
- A combination of tissue reconstruction and implants.
Breast reconstruction is a complex procedure performed by a plastic surgeon, also called a reconstructive surgeon. If you're planning breast reconstruction at the same time as a mastectomy, you'll meet with the plastic surgeon before the surgery. The plastic surgeon will coordinate with the breast surgeon to be available at the time of surgery.
Before surgery, you may need to consider whether you'll have radiation therapy afterward. Radiation therapy may impact your breast reconstruction options. Some people know they will need radiation as part of their treatment plan. Others may not know whether they need radiation until after the results of the mastectomy are known. You may meet with a radiation oncologist before or after surgery to discuss benefits and risks.
Preparing for your surgery
Your healthcare team will give you instructions before surgery. You may need to:
- Tell your healthcare team about any medicines, vitamins or supplements you're taking. Some substances could interfere with the surgery.
- Stop taking aspirin or other blood-thinning medicines. If you take blood thinners, your healthcare team will tell you when to stop taking these medicines. Sometimes a different blood-thinning medicine is given around the time of surgery.
- Stop eating before surgery. You'll receive specific instructions from your healthcare team about eating. You may need to stop eating several hours before surgery. You may be given the OK to drink liquids up to a certain time before surgery. Follow the instructions from your healthcare team.
- Make a plan for after surgery. Ask your healthcare team if you'll need to stay in the hospital. Most people go home the same day. Plan for a ride if you're told you can go home the same day. If you need to stay in the hospital another day, bring a robe and slippers to help make you more comfortable. Pack a bag with your toiletries and something to help you pass the time, such as a book.
What you can expect
Sentinel node biopsy
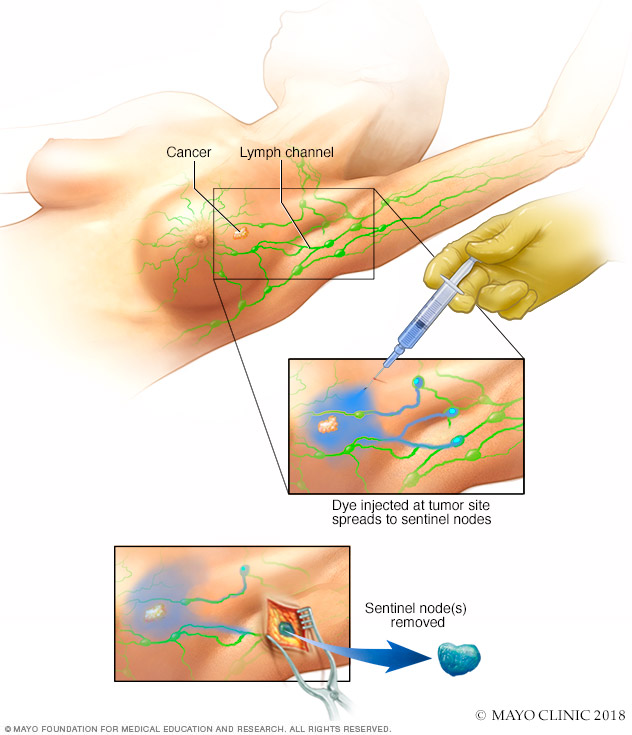
Sentinel node biopsy
Sentinel node biopsy identifies the first few lymph nodes into which a tumor drains. The surgeon uses a harmless dye and a weak radioactive solution to locate the sentinel nodes. The nodes are removed and tested for signs of cancer.
Mastectomy is a general term for the surgical removal of one or both breasts. Different types of mastectomies use different techniques. Many factors go into choosing what type of mastectomy is best for you. Types of mastectomies include:
- Total mastectomy. A total mastectomy, also known as a simple mastectomy, involves removing the entire breast, including the breast tissue, areola and nipple.
- Skin-sparing mastectomy. A skin-sparing mastectomy involves removing the breast tissue, nipple and areola, but not the breast skin. Breast reconstruction can be performed immediately after the mastectomy.
- Nipple-sparing mastectomy. A nipple- or areola-sparing mastectomy involves removing the breast tissue only, sparing the skin, nipple and areola. Breast reconstruction is performed immediately afterward.
If you're having a mastectomy to treat cancer, the surgeon also may remove nearby lymph nodes. When breast cancer spreads, it often goes to the lymph nodes first. Operations to remove lymph nodes include:
- Sentinel node biopsy. In a sentinel lymph node biopsy, the surgeon removes the first few nodes into which a cancer drains, called the sentinel nodes. These nodes are found using a radioactive tracer and dye injected on the day before surgery or on the day of surgery.
- Axillary node dissection. During an axillary node dissection, the surgeon removes all the lymph nodes from the armpit.
Lymph nodes removed during a mastectomy are tested for cancer. If no cancer is present, no more lymph nodes need be removed. If cancer is present, you may need additional treatment after surgery.
Before the procedure
A member of your healthcare team will tell you when and where to arrive for surgery. If other preparation is needed, you may start in one area and move to another area for surgery. A mastectomy without reconstruction usually takes 1 to 3 hours. The surgery is often done as an outpatient procedure. Most people go home on the same day of the operation.
If you're having a sentinel node biopsy, the radioactive tracer and blue dye are injected into the skin near the cancer before your surgery. The tracer and the dye travel to the sentinel nodes. This allows your surgeon to find the nodes and remove them during surgery.
During the procedure
A mastectomy is usually performed under general anesthesia. This means you're in a sleep-like state during the surgery. The surgeon starts by making an incision around your breast. The breast tissue is removed. Depending on your procedure, other parts of the breast also may be removed. The breast tissue and lymph nodes that are removed will be sent to a lab for testing.
If you're having breast reconstruction at the same time as a mastectomy, the plastic surgeon will do the reconstruction once the mastectomy is complete.
As the surgery is completed, the incision is closed with stitches. Often these stitches are the type that dissolve over time. Sometimes the stitches need to be removed at a follow up appointment. You might have one or two small plastic tubes placed where your breast was removed. The tubes drain any fluids that collect after surgery. The tubes are sewn into place, and the ends are attached to a small drainage bag.
After the procedure
Most people go home the same day of surgery. Some may need more time to recover and may stay overnight in the hospital.
After your surgery, you can expect to:
- Be taken to a recovery room where your blood pressure, pulse and breathing are monitored.
- Have a bandage over the surgery site.
- Feel some pain, numbness and a pinching feeling in your underarm area.
- Receive instructions on how to care for yourself at home. Instructions include taking care of your incision and drains, knowing signs of infection, and understanding activity restrictions.
- Talk with your healthcare team about when to wear a bra or wear a breast prosthesis.
- Be given prescriptions for pain medicine and possibly an antibiotic.
Results
After surgery the breast tissue and lymph nodes are sent to a lab for testing. Results from the lab will show whether all the cancer was removed and whether cancer was found in the lymph nodes. The results are typically available within a week or two after surgery. Your healthcare team will explain what the results mean and what the next steps will be in your treatment.
If you need more treatment, you may be referred to:
- A radiation oncologist to discuss radiation treatments. Radiation may be recommended for large cancers or for lymph nodes that test positive for cancer. Radiation also may be recommended for cancer that spreads into the skin, nipple or muscle, or for cancer that remains after the mastectomy.
- A medical oncologist to discuss other forms of treatment after the operation. These may include hormone therapy if your cancer is sensitive to hormones or chemotherapy or both.
- A plastic surgeon if you're considering breast reconstruction.
- A counselor or support group to help you cope with having breast cancer.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
The Mayo Clinic experience and patient stories
Our patients tell us that the quality of their interactions, our attention to detail and the efficiency of their visits mean health care like they've never experienced. See the stories of satisfied Mayo Clinic patients.

How a different mammogram experience led to lifesaving cancer diagnosis
Melissa Neuman dreaded getting mammograms. Her small, dense breasts made the screening exceptionally uncomfortable and painful. So Melissa put off getting an annual mammogram until she felt she couldn't delay any longer. For about five years, Melissa had been plagued with a nagging pain just under her left breast. In February 2023, a recommendation from a friend led her to seek care from Jessica Johnson, an OB-GYN nurse practitioner with Mayo Clinic Health System in Owatonna, Minnesota. "She took me seriously,…

Goldilocks surgery: Finding the perfect balance in breast cancer reconstruction
Kathleen Stewart was used to waiting for test results. She'd been called back for additional mammogram images many times and had already undergone two biopsies of suspicious areas in her breasts. In March 2022, as she waited for a call about the results of a breast biopsy, the resident of La Crosse, Wisconsin, felt she already knew what they would be. "I had already had that internal conversation that if I was diagnosed, I knew…