Overview
A living-donor transplant is a surgical procedure to remove an organ or portion of an organ from a living person and place it in another person whose organ is no longer functioning properly.
The popularity of living-organ donation has increased dramatically in recent years as an alternative to deceased-organ donation due to the growing need for organs for transplantation and shortage of available deceased-donor organs. More than 5,700 living-organ donations are reported each year in the United States.
Living-kidney donation is the most common type of living-donor transplant. Individuals can donate one of their two kidneys. The remaining kidney is able to perform necessary functions.
Living donors can also donate a portion of their livers. The remaining liver regenerates, grows back to nearly its original size and performs its typical functions.
Kidney and liver transplants are the most common types of living-donor organ procedures. However, living people may also donate tissues for transplantation — such as skin, bone marrow and blood-forming cells.
Start your donor evaluation
Begin the process of becoming a living kidney or liver donor by clicking here to complete a health history questionnaire.
Living-organ donation types
There are two types of living-organ donation.
Directed donation
This is the most common type of living-donor organ donation. In this type, the donor directs the organ to a specific recipient for transplant.
The donor may be:
- A first-degree relative, such as a parent, brother, sister or adult child
- Other blood relatives such as uncles, aunts or cousins
- A biologically unrelated person who has a connection with the transplant candidate, such as a spouse or significant other, a friend, or a co-worker
- A person who has heard about the transplant candidate's need
Nondirected donation
In nondirected living-donor organ donation, also known as good Samaritan or altruistic donation, the donor does not name the recipient of the donated organ. The match is based on medical need and blood type compatibility.
In some cases, the donor may choose not to know the organ recipient. In other cases, the donor and recipient may meet if both agree and if the transplant center policy allows it.
Paired-organ donation and donation chains
Paired organ donation

Paired organ donation
In paired organ donation, living donors and their recipients aren't compatible for a transplant. However, the donor of each pair is compatible with the recipient of the other pair. If both donors and recipients are willing, your healthcare team may consider a paired donation.
Living-donor organ donation chain
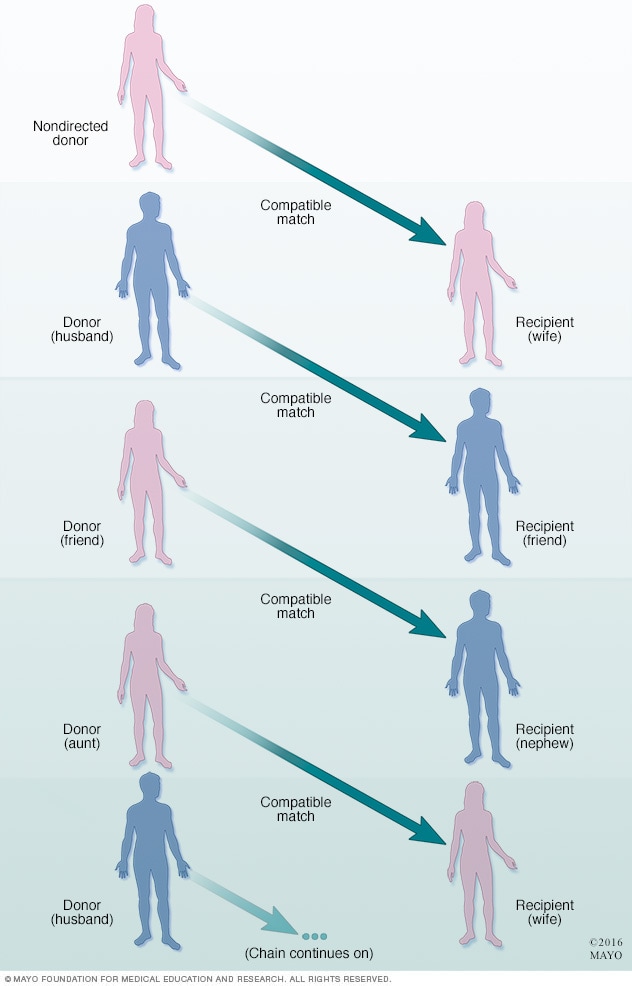
Living-donor organ donation chain
More than one pair of living donors and recipients who are not compatible may be linked with a nondirected living donor to form a donation chain in order to receive compatible organs.
Living donors often play an important role in paired-organ donation and donation chains. Paired-organ donation (also known as paired exchange) may be an option when a donor and intended recipient have incompatible blood types. Paired-organ donation may also be an option when the recipient has certain antibodies that will react to the donor's cells, which could cause the transplant to fail.
In paired-organ donation, two or more organ-recipient pairs trade donors so that each recipient gets an organ that is compatible with his or her blood type. A nondirected living donor may also participate in paired-organ donation to help match incompatible pairs.
More than one pair of incompatible living donors and recipients may be linked with a nondirected living donor to form a donation chain in order to receive compatible organs. In this scenario, multiple recipients benefit from a single nondirected living donor.
Products & Services
Types
Why it's done
Living-donor transplantation offers an alternative to waiting for a deceased-donor organ to become available for people in need of an organ transplant.
In addition, living-donor organ transplants are associated with fewer complications than are deceased-donor transplants and, overall, a longer survival of the donor organ.
Risks
The risks associated with living-donor organ donation include both short- and long-term health risks of the surgical procedures, problems with a donor's remaining organ function, and psychological problems following organ donation.
For the organ recipient, the risk of transplant surgery is usually low because it is a potentially lifesaving procedure. But for the donor, organ donation can expose a healthy person to the risk of and recovery from unnecessary major surgery.
Immediate, surgery-related risks of organ donation include pain, infection, hernia, bleeding, blood clots, wound complications and, in rare cases, death.
Long-term follow-up information on living-organ donors is limited, and studies are ongoing. Overall, available data shows that organ donors fare very well over the long term.
Donating an organ may also cause mental health issues, such as symptoms of anxiety and depression. The donated organ may not work properly in the recipient and cause feelings of regret, anger or resentment in the donor.
The known health risks associated with living-organ donation vary according to the type of donation. To minimize risks, donors need to have extensive testing to ensure they're eligible to donate.
Kidney donation risks
Living-donor kidney transplant is the most widely studied type of living-organ donation, with more than 50 years of follow-up information. Overall, studies show that the life expectancy of those who have donated a kidney is the same as that of similarly matched people who haven't.
Some studies suggest that living kidney donors may have a slightly higher risk of kidney failure in the future. But this risk is still smaller than the average risk of kidney failure in the general population. Specific long-term complications associated with living-kidney donation include high blood pressure, elevated protein levels in urine and reduced kidney function.
Liver donation risks
The risks of living liver donation also are low, but experience with this procedure is more limited because it was introduced into medical practice more recently than kidney donation. The first living-donor liver transplant was performed in 1989.
Living liver donation may also cause bile leakage, narrowing of the bile duct, intra-abdominal bleeding and, in rare cases, inadequate growth of the remaining part of the liver.
How you prepare
Making an informed decision
The decision to donate an organ is a personal one that deserves careful thought and consideration of both the serious risks and the benefits. Talk through your decision with your friends, family and other trusted advisers.
You should not feel pressured to donate, and you may change your mind at any point.
Some helpful questions to consider:
- How do I feel about organ donation?
- What are the medical risks?
- What will my insurance cover?
- How will donating affect me financially or my ability to work?
- Do I know enough to make an informed decision?
- Is someone pressuring me psychologically to be a living donor?
- How will donating or not donating affect my relationship with the recipient?
- Is there someone else who could donate?
- If there is more than one possible donor, how will the living donor be chosen?
- How does my religion view organ donation?
- Are there aspects of my health or medical history that I know should keep me from donating?
- Do I have a support network in place to help me through this process?
- How will I feel if I'm rejected during the evaluation process?
- How will I feel if my recipient does not do well after the transplant?
Your medical information is kept confidential by the transplant center. If you are rejected as a donor during the evaluation process, the donor is told only that your organ was declined. It is up to you whether you tell the recipient (if known) the reason.
The Centers for Medicare & Medicaid Services and the Organ Procurement and Transplantation Network (OPTN) require that living-donor transplant centers provide an independent living-donor advocate to protect the informed consent process. This advocate is often a social worker or counselor who can help you discuss your feelings, answer any questions you have and assist in protecting your best interests throughout the donation process.
Choosing a transplant center
Your health care provider or your recipient's physician may recommend a transplant center for your procedure. You're also free to select a transplant center on your own or choose a center from your insurance company's list of preferred providers.
When considering a transplant center, you may want to:
- Learn about the number and type of transplants the center performs each year
- Ask about the transplant center's organ donor and recipient survival rates
- Compare transplant center statistics through the database maintained by the Scientific Registry of Transplant Recipients
- Assess the center's commitment to keeping up with the latest transplant technology and techniques, which indicates that the program is growing
- Consider other services provided by the transplant center, such as support groups, travel arrangements, local housing for your recovery period and referrals to other resources
If you're committed to donating an organ, your transplant team will partner with you and your doctor throughout the living-donor transplantation process.
What you can expect
Before the procedure
Donor evaluation
If possible, bring a family member or friend with you for your evaluation. It may be helpful for you to discuss your decision to donate with someone you trust.
Living-organ donors are generally between the ages of 18 and 60 and in good physical and mental health. Specific living-donor eligibility standards vary by organ and transplant center.
The donor evaluation process usually includes the following steps:
- Initial screening. The first step in living-donor evaluation is usually an initial screening, which may be completed online, in person or over the phone. The transplant center staff will ask for your consent to begin a medical screening and ask several questions about your health and medical history.
- Blood tests. The next step is usually a blood test to determine if your blood type is compatible with the recipient's. If your blood type doesn't match your intended recipient, there may be specialized medical treatment alternatives that still allow you to donate.
-
Physical examination and psychological evaluation. At the transplant center, a transplant team will evaluate your general physical and mental health to make sure that undergoing living-donor surgery will pose minimal risks to you.
Doctors will perform tests to look for preexisting conditions that may disqualify you from being a donor, such as diabetes, cancer, some infectious diseases, heart diseases or other conditions.
If you are participating in directed donation, different transplant team members will perform evaluations and surgeries for you and your recipient. Your evaluation is confidential.
Also, during the evaluation, the team will check to ensure that the organ you're planning to donate is healthy and that removing either one of your kidneys or a portion of your liver is unlikely to cause health problems later in life. This part of the evaluation may include laboratory and imaging tests.
-
Consent and final review. If you meet eligibility requirements to be a living donor, the transplant center is required to inform you of all aspects and potential results of organ donation and receive your informed consent to the procedure.
Transplant staff will discuss with you and your family the benefits and risks of donating a kidney or a portion of your liver and answer your questions. Staff will also discuss the importance of maintaining a healthy lifestyle before and after donating an organ.
During the procedure
Living kidney donor laparoscopic nephrectomy
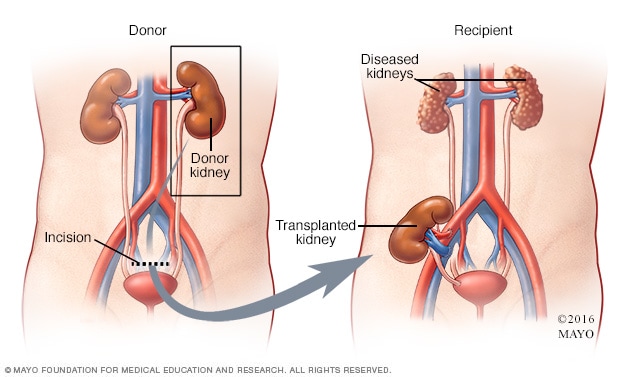
Living kidney donor laparoscopic nephrectomy
In a laparoscopic nephrectomy, the surgeon makes two or three small incisions close to the bellybutton and uses a special camera called a laparoscope to view the internal organs and guide the procedure. The donor kidney is then removed and transplanted into the recipient.
Living kidney donation
Most procedures to remove a living donor's kidney for a transplant are done through minimally invasive surgery (laparoscopic nephrectomy). Laparoscopic nephrectomy involves less pain and a shorter recovery compared with traditional open surgery to remove a kidney (open nephrectomy).
In a laparoscopic nephrectomy, the surgeon makes two or three small incisions close to the bellybutton and uses a special camera called a laparoscope to view the internal organs and guide the surgeon through the procedure.
In some cases, donors may not qualify for minimally invasive surgery, and may need to have an open nephrectomy. This may be the case if donors have had multiple abdominal surgeries or if they are significantly overweight.
In open nephrectomy, a 5- to 7-inch incision is made on the side of the chest and upper abdomen. The surgeon then uses a surgical instrument called a retractor to spread the ribs to access the donor's kidney.
Both open and laparoscopic nephrectomy last about 2 to 3 hours, and are performed using general anesthesia, which means you'll be asleep during the entire surgery.
Living liver transplant
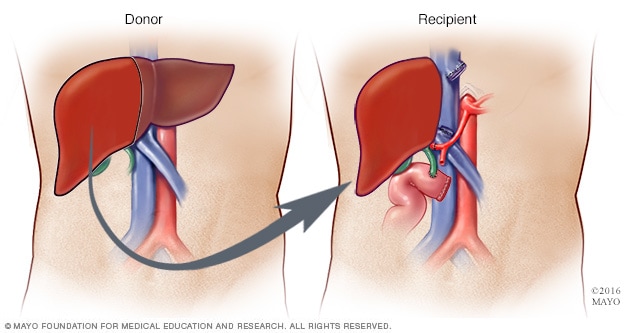
Living liver transplant
During living liver donation, surgeons remove about 40% to 70% of the donor liver and place it into the recipient.
Living liver donor organ regeneration

Living liver donor organ regeneration
Within the first week after living liver donor surgery, the donor's liver starts to grow back to its typical size. Standard liver volume returns within about two months after donation.
Living liver donation
During living liver donation, surgeons remove a portion of the liver through an incision in the abdomen.
Either the left or right lobe of the liver may be used in donation, depending on the size of the recipient.
About 40% to 70% of the donor's liver is removed for transplantation. The donor's liver begins to regrow almost immediately after surgery, reaching normal size and volume again within about two months after donation.
The surgery is performed under general anesthesia and can last up to 10 hours.
After the procedure
- Hospital stay. You'll stay in the hospital for a few days after kidney donation and up to seven days after liver donation.
-
Care after your surgery. If you live far from your transplant center, your doctors will recommend that you stay close to the center for a few days after you leave the hospital so that they can monitor your health and remaining organ function.
You'll likely need to return to your transplant center for follow-up care, tests and monitoring several times after your surgery. Transplant centers are required to submit follow-up data at six months, 12 months and 24 months after donation. Your local health care provider may conduct your laboratory tests one and two years after your kidney or liver surgery.
- Recovery. Depending on your living-donor procedure and overall health, a member of your transplant team will give you specific advice on how to take care of yourself and reduce the risk of complications during your recovery, including caring for your incision, managing pain, limiting strenuous activities and returning to your typical diet.
-
Return to regular activities. After donating a kidney, most people are able to return to their typical daily activities after 4 to 6 weeks.
The recovery process takes a little longer for liver donation, and most people are able to return to work and other regular activities 2 to 3 months after donation.
-
Pregnancy. Kidney donation normally does not affect the ability to become pregnant or complete a safe pregnancy and childbirth. Some studies suggest that kidney donors may have a small increase in risk of pregnancy complications such as gestational diabetes, pregnancy-induced hypertension, preeclampsia and protein in the urine.
It's usually recommended that women wait at least six months after living kidney donation before becoming pregnant.
Little is known about pregnancy after living liver donation since the procedure is newer and less common.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Coping and Support
Donating an organ is a personal decision that requires careful thought and consideration of both the serious risks and the benefits. Talk through your decision with your friends, family and other trusted advisers.
Your transplant team also can assist you with other useful resources and coping strategies throughout the organ donation process, such as:
- Joining a support group for organ donors. Talking with others who have shared your experience can ease fears and anxiety.
- Sharing your experiences on social media. Engaging with others who have had a similar experience may help you set realistic expectations before you make a decision.
- Educating yourself. Learn as much as you can about your procedure and ask questions about things you don't understand. Knowledge is empowering.
Diet and nutrition
You should be able to go back to your typical diet soon after your living-donation surgery. Unless you have other health issues, you won't likely have any specific dietary restrictions related to your procedure.
Your transplant team includes a dietitian who can discuss your nutrition and diet needs and answer any questions you have after your surgery.
Exercise
Maintaining a healthy lifestyle through diet and exercise is just as important for living organ donors as it is for everyone else.
You will likely be able to return to your typical physical activity levels within a few weeks or months after living-donor surgery. Your transplant team can discuss your individual physical activity goals and needs with you.
It's important to talk with your health care provider before starting any new physical activity.
Some doctors recommend the living kidney donors protect the remaining kidney by avoiding contact sports, such as football, boxing, hockey, soccer, martial arts or wrestling. Wearing protective gear such as padded vests under clothing to protect the kidney from injury during sports also may be recommended.
Jan. 31, 2025