Overview
In vitro fertilization
In vitro fertilization
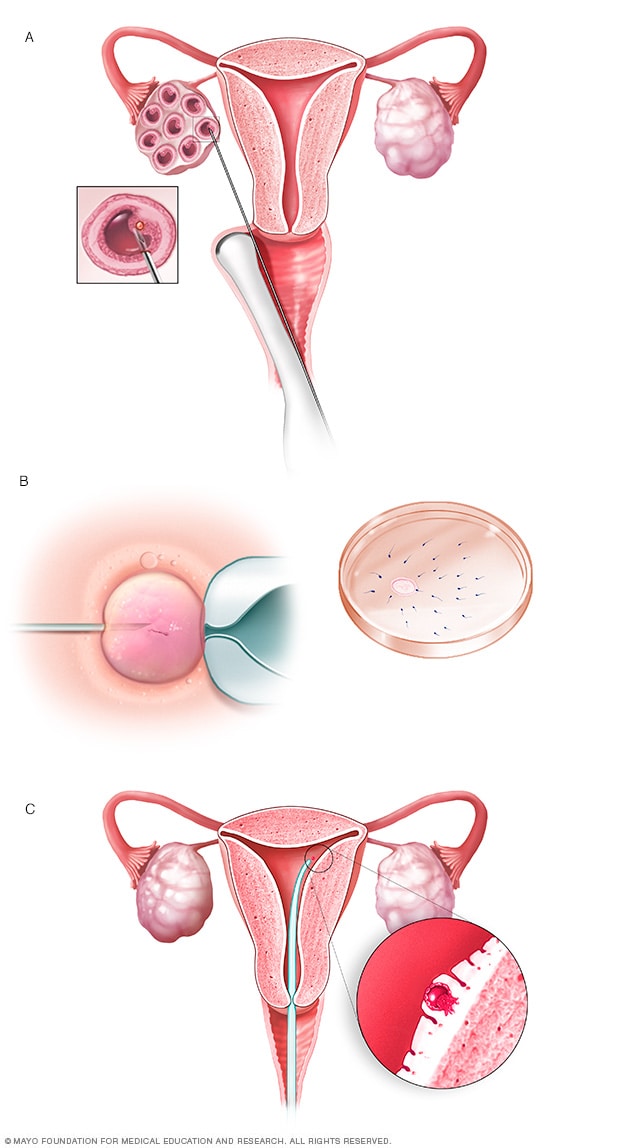
During in vitro fertilization, eggs are removed from sacs called follicles within an ovary (A). An egg is fertilized by injecting a single sperm into the egg or mixing the egg with sperm in a petri dish (B). The fertilized egg, called an embryo, is transferred into the uterus (C).
In vitro fertilization, also called IVF, is a complex series of procedures that can lead to a pregnancy. It's a treatment for infertility, a condition in which you can't get pregnant after at least a year of trying for most couples. IVF also can be used to prevent passing on genetic problems to a child.
During in vitro fertilization, mature eggs are collected from ovaries and fertilized by sperm in a lab. Then a procedure is done to place one or more of the fertilized eggs, called embryos, in a uterus, which is where babies develop. One full cycle of IVF takes about 2 to 3 weeks. Sometimes these steps are split into different parts and the process can take longer.
In vitro fertilization is the most effective type of fertility treatment that involves the handling of eggs or embryos and sperm. Together, this group of treatments is called assisted reproductive technology.
IVF can be done using a couple's own eggs and sperm. Or it may involve eggs, sperm or embryos from a known or unknown donor. In some cases, a gestational carrier — someone who has an embryo implanted in the uterus — might be used.
Your chances of having a healthy baby using IVF depend on many factors, such as your age and the cause of infertility. What's more, IVF involves getting procedures that can be time-consuming, expensive and invasive. If more than one embryo is placed in the uterus, it can result in a pregnancy with more than one baby. This is called a multiple pregnancy.
Your health care team can help you understand how IVF works, what the risks are and whether it's right for you.
Products & Services
Why it's done
In vitro fertilization is a treatment for infertility or genetic problems. Before you have IVF to treat infertility, you and your partner might be able to try other treatment options that involve fewer or no procedures that enter the body. For example, fertility drugs can help the ovaries make more eggs. And a procedure called intrauterine insemination places sperm directly in the uterus near the time when an ovary releases an egg, called ovulation.
Sometimes, IVF is offered as a main treatment for infertility in people over the age of 40. It also can be done if you have certain health conditions. For example, IVF may be an option if you or your partner has:
- Fallopian tube damage or blockage. Eggs move from the ovaries to the uterus through the fallopian tubes. If both tubes get damaged or blocked, that makes it hard for an egg to be fertilized or for an embryo to travel to the uterus.
- Ovulation disorders. If ovulation doesn't happen or doesn't occur often, fewer eggs are available to be fertilized by sperm.
- Endometriosis. This condition happens when tissue that's like the lining of the uterus grows outside of the uterus. Endometriosis often affects the ovaries, uterus and fallopian tubes.
- Uterine fibroids. Fibroids are tumors in the uterus. Most often, they're not cancer. They're common in people in their 30s and 40s. Fibroids can cause a fertilized egg to have trouble attaching to the lining of the uterus.
- Previous surgery to prevent pregnancy. An operation called tubal ligation involves having the fallopian tubes cut or blocked to prevent pregnancy for good. If you wish to conceive after tubal ligation, IVF may help. It might be an option if you don't want or can't get surgery to reverse tubal ligation.
- Issues with sperm. A low number of sperm or unusual changes in their movement, size or shape can make it hard for sperm to fertilize an egg. If medical tests find issues with sperm, a visit to an infertility specialist might be needed to see if there are treatable problems or other health concerns.
- Unexplained infertility. This is when tests can't find the reason for someone's infertility.
- A genetic disorder. If you or your partner is at risk of passing on a genetic disorder to your child, your health care team might recommend getting a procedure that involves IVF. It's called preimplantation genetic testing. After the eggs are harvested and fertilized, they're checked for certain genetic problems. Still, not all of these disorders can be found. Embryos that don't appear to contain a genetic problem can be placed in the uterus.
-
A desire to preserve fertility due to cancer or other health conditions. Cancer treatments such as radiation or chemotherapy can harm fertility. If you're about to start treatment for cancer, IVF could be a way to still have a baby in the future. Eggs can be harvested from their ovaries and frozen for later use. Or the eggs can be fertilized and frozen as embryos for future use.
People who don't have a working uterus or for whom pregnancy poses a serious health risk might choose IVF using another person to carry the pregnancy. The person is called a gestational carrier. In this case, your eggs are fertilized with sperm, but the embryos that result are placed in the gestational carrier's uterus.
Risks
IVF raises the chances of certain health problems. From short term to longer term, these risks include:
- Stress. IVF can be draining for the body, mind and finances. Support from counselors, family and friends can help you and your partner through the ups and downs of infertility treatment.
- Complications from the procedure to retrieve eggs. After you take medicines to spur the growth of sacs in the ovaries that each contain an egg, a procedure is done to collect the eggs. This is called egg retrieval. Ultrasound images are used to guide a long, thin needle through the vagina and into the sacs, also called follicles, to harvest the eggs. The needle could cause bleeding, infection or damage to the bowel, bladder or a blood vessel. Risks are also linked with medicines that can help you sleep and prevent pain during the procedure, called anesthesia.
-
Ovarian hyperstimulation syndrome. This is a condition in which the ovaries become swollen and painful. It can be caused by receiving shots of fertility medicines, such as human chorionic gonadotropin (HCG), to trigger ovulation.
Symptoms often last up to a week. They include mild belly pain, bloating, upset stomach, vomiting and diarrhea. If you become pregnant, your symptoms might last a few weeks. Rarely, some people get a worse form of ovarian hyperstimulation syndrome that also can cause rapid weight gain and shortness of breath.
- Miscarriage. The rate of miscarriage for people who conceive using IVF with fresh embryos is similar to that of people who conceive naturally — about 15% for pregnant people in their 20s to over 50% for those in their 40s. The rate rises with the pregnant person's age.
- Ectopic pregnancy. This is a condition in which a fertilized egg attaches to tissue outside the uterus, often in a fallopian tube. The embryo can't survive outside the uterus, and there's no way to continue the pregnancy. A small percentage of people who use IVF will have an ectopic pregnancy.
- Multiple pregnancy. IVF raises the risk of having more than one baby. Becoming pregnant with multiple babies carries higher risks of pregnancy-related high blood pressure and diabetes, early labor and delivery, low birth weight, and birth defects than does pregnancy with a single baby.
- Birth defects. The age of the mother is the main risk factor for birth defects, no matter how the child is conceived. But assisted reproductive technologies such as IVF are linked with a slightly higher risk of a baby being born with heart issues, digestive problems or other conditions. More research is needed to find out if it's IVF that causes this raised risk or something else.
- Premature delivery and low birth weight. Research suggests that IVF slightly raises the risk that the baby will be born early or with a low birth weight.
- Cancer. Some early studies suggested that certain medicines used to stimulate egg growth might be linked with getting a specific type of ovarian tumor. But more-recent studies do not support these findings. There doesn't seem to be a significantly higher risk of breast, endometrial, cervical or ovarian cancer after IVF.
How you prepare
To get started, you'll want to find a reputable fertility clinic. If you live in the United States, the Centers for Disease Control and Prevention and the Society for Assisted Reproductive Technology provide information online about clinics' individual pregnancy and live birth rates.
A fertility clinic's success rate depends on many things. These include the ages and medical issues of people they treat, as well as the clinic's treatment approaches. When you talk with a representative at a clinic, also ask for detailed information about the costs of each step of the procedure.
Before you start a cycle of IVF using your own eggs and sperm, you and your partner will likely need various screening tests. These include:
- Ovarian reserve testing. This involves getting blood tests to find out how many eggs are available in the body. This is also called egg supply. The results of the blood tests, often used together with an ultrasound of the ovaries, can help predict how your ovaries will respond to fertility medicines.
- Semen analysis. Semen is the fluid that contains sperm. An analysis of it can check the amount of sperm, their shape and how they move. This testing may be part of an initial fertility evaluation. Or it might be done shortly before the start of an IVF treatment cycle.
- Infectious disease screening. You and your partner will both be screened for diseases such as HIV.
- Practice embryo transfer. This test doesn't place a real embryo in the uterus. It may be done to figure out the depth of your uterus. It also helps determine the technique that's most likely to work well when one or more actual embryos are inserted.
- Uterine exam. The inside lining of the uterus is checked before you start IVF. This might involve getting a test called sonohysterography. Fluid is sent through the cervix into the uterus using a thin plastic tube. The fluid helps make more-detailed ultrasound images of the uterine lining. Or the uterine exam might include a test called hysteroscopy. A thin, flexible, lighted telescope is inserted through the vagina and cervix into the uterus to see inside it.
Before you begin a cycle of IVF, think about some key questions, including:
-
How many embryos will be transferred? The number of embryos placed in the uterus often is based on age and the number of eggs collected. Since the rate of fertilized eggs attaching to the lining of uterus is lower for older people, usually more embryos are transferred — except for people who use donor eggs from a young person, genetically tested embryos or in certain other cases.
Most health care professionals follow specific guidelines to prevent a multiple pregnancy with triplets or more. In some countries, legislation limits the number of embryos that can be transferred. Make sure you and your care team agree on the number of embryos that will be placed in the uterus before the transfer procedure.
-
What will you do with any extra embryos? Extra embryos can be frozen and stored for future use for many years. Not all embryos will survive the freezing and thawing process, but most will.
Having frozen embryos can make future cycles of IVF less expensive and less invasive. Or you might be able to donate unused frozen embryos to another couple or a research facility. You also might choose to discard unused embryos. Make sure you feel comfortable making decisions about extra embryos before they are created.
- How will you handle a multiple pregnancy? If more than one embryo is placed in your uterus, IVF can cause you to have a multiple pregnancy. This poses health risks for you and your babies. In some cases, a surgery called fetal reduction can be used to help a person deliver fewer babies with lower health risks. Getting fetal reduction is a major decision with ethical, emotional and mental risks.
- Have you thought through the risks linked with using donor eggs, sperm or embryos, or a gestational carrier? A trained counselor with expertise in donor issues can help you understand the concerns, such as the legal rights of the donor. You also may need an attorney to file court papers to help you become legal parents of an embryo that's developing in the uterus.
What you can expect
After the preparations are completed, one cycle of IVF can take about 2 to 3 weeks. More than one cycle may be needed. The steps in a cycle go as follows:
Treatment to make mature eggs
The start of an IVF cycle begins by using lab-made hormones to help the ovaries to make eggs — rather than the single egg that usually develops each month. Multiple eggs are needed because some eggs won't fertilize or develop correctly after they're combined with sperm.
Certain medicines may be used to:
- Stimulate the ovaries. You might receive shots of hormones that help more than one egg develop at a time. The shot may contain a follicle-stimulating hormone (FSH), a luteinizing hormone (LH) or both.
- Help eggs mature. A hormone called human chorionic gonadotropin (HCG), or other medicines, can help the eggs ripen and get ready to be released from their sacs, called follicles, in the ovaries.
- Delay ovulation. These medicines prevent the body from releasing the developing eggs too soon.
- Prepare the lining of the uterus. You might start to take supplements of the hormone progesterone on the day of the procedure to collect your eggs. Or you might take these supplements around the time an embryo is placed in the uterus. They improve the odds that a fertilized egg attaches to the lining of your uterus.
Your doctor decides which medicines to use and when to use them.
Most often, you'll need 1 to 2 weeks of ovarian stimulation before your eggs are ready to be collected with the egg retrieval procedure. To figure out when the eggs are ready, you may need:
- Vaginal ultrasound, an imaging exam of the ovaries to track the developing follicles. Those are the fluid-filled sacs in the ovaries where eggs mature.
- Blood tests, to check on how you respond to ovarian stimulation medicines. Estrogen levels often rise as follicles develop. Progesterone levels remain low until after ovulation.
Sometimes, IVF cycles need to be canceled before the eggs are collected. Reasons for this include:
- Not enough follicles develop.
- Ovulation happens too soon.
- Too many follicles develop, raising the risk of ovarian hyperstimulation syndrome.
- Other medical issues happen.
If your cycle is canceled, your care team might recommend changing medicines or the amounts you take, called doses. This might lead to a better response during future IVF cycles. Or you may be advised that you need an egg donor.
Egg retrieval
This is the procedure to collect the eggs from one or both ovaries. It takes place in your doctor's office or a clinic. The procedure is done 34 to 36 hours after the final shot of fertility medicine and before ovulation.
- Before egg retrieval, you'll be given medicine to help you relax and keep you from feeling pain.
- An ultrasound device is placed into the vagina to find follicles. Those are the sacs in the ovaries that each contain an egg. Then a thin needle is inserted into an ultrasound guide to go through the vagina and into the follicles to collect the eggs. This process is called transvaginal ultrasound aspiration.
- If your ovaries can't be reached through the vagina this way, an ultrasound of the stomach area may be used to guide the needle through the stomach and into the ovaries.
- The eggs are removed from the follicles through a needle connected to a suction device. Multiple eggs can be removed in about 20 minutes.
- After the procedure, you may have cramping and feelings of fullness or pressure.
- Mature eggs are placed in a liquid that helps them develop. Eggs that appear healthy and mature will be mixed with sperm to attempt to create embryos. But not all eggs are able to be fertilized with success.
Sperm retrieval
If you're using your partner's sperm, a semen sample needs to be collected at your doctor's office or clinic the morning of egg retrieval. Or sperm can be collected ahead of time and frozen.
Most often, the semen sample is collected through masturbation. Other methods can be used if a person can't ejaculate or has no sperm in the semen. For example, a procedure called testicular aspiration uses a needle or surgery to collect sperm directly from the testicle. Sperm from a donor also can be used. Sperm are separated from the semen fluid in the lab.
Fertilization
Two common methods can be used to try to fertilize eggs with sperm:
- Conventional insemination. Healthy sperm and mature eggs are mixed and kept in a controlled environment called an incubator.
- Intracytoplasmic sperm injection (ICSI). A single healthy sperm is injected right into each mature egg. Often, ICSI is used when semen quality or number is an issue. Or it might be used if fertilization attempts during prior IVF cycles didn't work.
In certain situations, other procedures may be recommended before embryos are placed in the uterus. These include:
-
Assisted hatching. About 5 to 6 days after fertilization, an embryo "hatches" from the thin layer that surrounds it, called a membrane. This lets the embryo attach to the lining of the uterus.
If you're older and you want to get pregnant, or if you have had past IVF attempts that didn't work, a technique called assisted hatching might be recommended. With this procedure, a hole is made in the embryo's membrane just before the embryo is placed in the uterus. This helps the embryo hatch and attach to the lining of the uterus. Assisted hatching is also useful for eggs or embryos that were frozen, as that process can harden the membrane.
-
Preimplantation genetic testing. Embryos are allowed to develop in the incubator until they reach a stage where a small sample can be removed. The sample is tested for certain genetic diseases or the correct number of threadlike structures of DNA, called chromosomes. There are usually 46 chromosomes in each cell. Embryos that don't contain affected genes or chromosomes can be transferred to the uterus.
Preimplantation genetic testing can lower the chances that a parent will pass on a genetic problem. It can't get rid of the risk completely. Prenatal testing may still be recommended during pregnancy.
Embryo transfer
Egg-retrieval technique
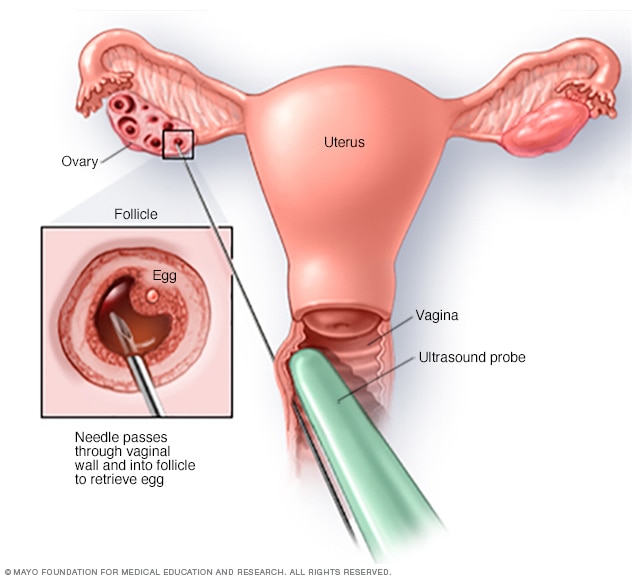
Egg-retrieval technique
Typically, transvaginal ultrasound aspiration is used to retrieve eggs. During this procedure, an ultrasound probe is inserted into the vagina to identify follicles. A needle is guided through the vagina and into the follicles. The eggs are removed from the follicles through the needle, which is connected to a suction device.
ICSI
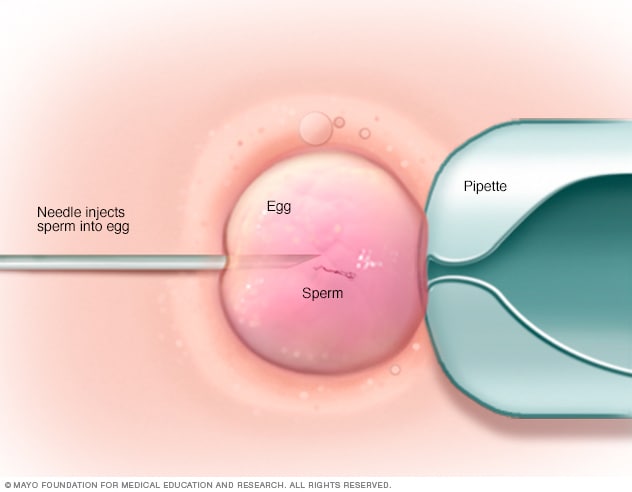
ICSI
In intracytoplasmic sperm injection (ICSI), a single healthy sperm is injected directly into each mature egg. ICSI often is used when semen quality or number is a problem or if fertilization attempts during prior in vitro fertilization cycles failed.
Blastocyst
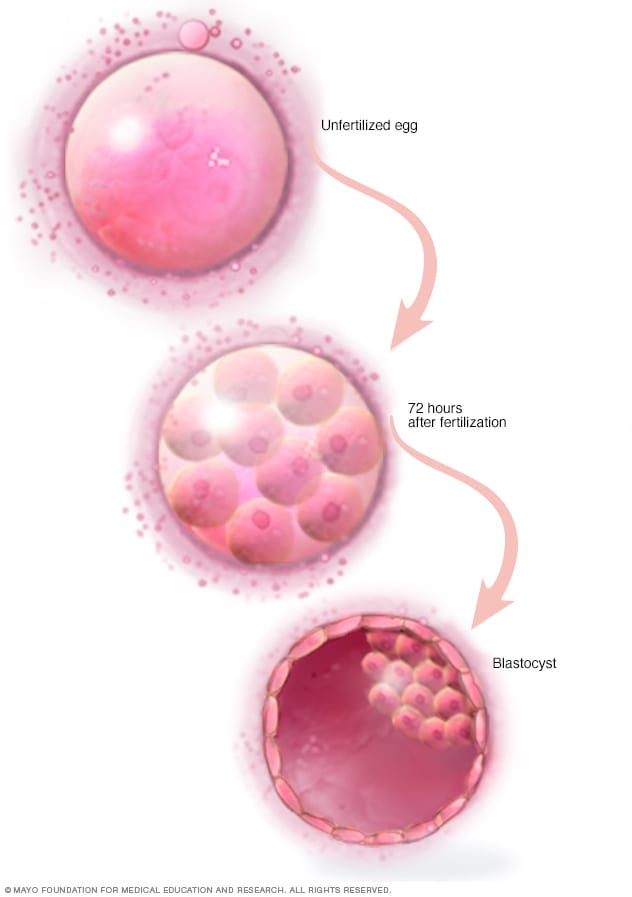
Blastocyst
Three days after fertilization, a healthy embryo will contain about 6 to 10 cells. By the fifth or sixth day, the fertilized egg is known as a blastocyst — a rapidly dividing ball of cells. The inner group of cells will become the embryo. The outer group will become the cells that nourish and protect it.
The procedure to place one or more embryos in the uterus is done at your doctor's office or a clinic. It often takes place 2 to 6 days after eggs are collected.
- You might be given a mild sedative to help you relax. The procedure is often painless, but you might have mild cramping.
- A long, thin, flexible tube called a catheter is placed into the vagina, through the cervix and into the uterus.
- A syringe that contains one or more embryos in a small amount of fluid is attached to the end of the catheter.
- Using the syringe, the embryo or embryos are placed into the uterus.
If the procedure works, an embryo will attach to the lining of your uterus about 6 to 10 days after egg retrieval.
After the procedure
After the embryo transfer, you can get back to your usual daily routine. Your ovaries may still be enlarged, so vigorous activities or sex might cause discomfort. Ask your care team how long you should stay away from these.
Typical side effects include:
- Passing a small amount of clear or bloody fluid shortly after the procedure. This is due to the swabbing of the cervix before the embryo transfer.
- Breast tenderness due to high estrogen levels.
- Mild bloating.
- Mild cramping.
- Constipation.
Call your care team if you have moderate or severe pain, or heavy bleeding from the vagina after the embryo transfer. You'll likely to need to get checked for complications such as infection, twisting of an ovary and ovarian hyperstimulation syndrome.
Results
At least 12 days after egg retrieval, you get a blood test to find out whether you're pregnant.
- If you're pregnant, you'll likely be referred to an obstetrician or other pregnancy specialist for prenatal care.
- If you're not pregnant, you'll stop taking progesterone and likely get your period within a week. Call your care team if you don't get your period or if you have unusual bleeding. If you'd like to try another cycle of IVF, your care team might suggest steps you can take to improve your chances of getting pregnant next time.
The chances of giving birth to a healthy baby after using IVF depend on various factors, including:
- Maternal age. The younger you are, the more likely you are to get pregnant and give birth to a healthy baby using your own eggs during IVF. Often, people 40 and older are counseled to think about using donor eggs during IVF to boost the chances of success.
- Embryo status. Transfer of embryos that are more developed is linked with higher pregnancy rates compared with less-developed embryos. But not all embryos survive the development process. Talk with your care team about your specific situation.
- Reproductive history. People who've given birth before are more likely to be able to get pregnant using IVF than are people who've never given birth. Success rates are lower for people who've already tried IVF multiple times but didn't get pregnant.
- Cause of infertility. Having an average supply of eggs raises your chances of being able to get pregnant using IVF. People who have severe endometriosis are less likely to be able to get pregnant using IVF than are those who have infertility without a clear cause.
- Lifestyle factors. Smoking can lower the chance of success with IVF. Often, people who smoke have fewer eggs retrieved during IVF and may miscarry more often. Obesity also can lower the chances of getting pregnant and having a baby. Use of alcohol, drugs, too much caffeine and certain medicines also can be harmful.
Talk with your care team about any factors that apply to you and how they may affect your chances of a successful pregnancy.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
The Mayo Clinic experience and patient stories
Our patients tell us that the quality of their interactions, our attention to detail and the efficiency of their visits mean health care like they've never experienced. See the stories of satisfied Mayo Clinic patients.

'What we were waiting for': Couple shares journey from infertility to joy
Jay, Charlotte, Thomas and Erin Barreto Erin Barreto, a pharmacist, reflects on years of infertility, resilience, healing and the joy of welcoming two children through IVF. "It was a long, uncertain road filled with setbacks around every corner. When you had those moments of hope, you had to hang on to them." Erin Barreto, Pharm.D., Ph.D., a Mayo Clinic pharmacist and now mom of two, spent nearly seven years navigating the complex path of infertility with the Reproductive…
Sept. 01, 2023