Overview
The human papillomavirus (HPV) test detects the presence of human papillomavirus, a virus that can lead to the development of genital warts, abnormal cervical cells or cervical cancer.
Your doctor may likely recommend the HPV test if:
- Your Pap test was abnormal, showing atypical squamous cells of undetermined significance (ASCUS)
- You're age 30 or older
The HPV test is only approved for cells from the cervix. A healthcare professional may suggest an HPV test for cells from other sites, such as the anus. HPV testing on anal cells is not recommended in general. But some people may benefit from screening, such as:
- Anyone age 35 or older who has HIV.
- People who have had high-risk HPV types detected on the penis, scrotum, cervix, vagina or vulva.
- Solid organ transplant recipients.
Why it's done
The HPV test is a screening test for cervical cancer, but the test doesn't tell you whether you have cancer. Instead, the test detects the presence of HPV, the virus that causes cervical cancer, in your system. Certain types of HPV — including types 16 and 18 — increase your cervical cancer risk.
Knowing whether you have a type of HPV that puts you at high risk of cervical cancer means that you and your doctor can better decide on the next steps in your health care. Those steps might include follow-up monitoring, further testing or treatment of abnormal cells.
Routine use of the HPV test under age 30 isn't recommended, nor is it very helpful. HPV spreads through sexual contact and is very common in young people — frequently, the test results will be positive. However, HPV infections often clear on their own within a year or two.
Cervical changes that lead to cancer usually take several years — often 10 years or more — to develop. For these reasons, you might follow a course of watchful waiting instead of undergoing treatment immediately.
Risks
As with any screening test, an HPV test carries the risk of false-positive or false-negative results.
- False-positive. A false-positive test result indicates that you have a high-risk type of HPV when you really don't. A false-positive result could lead to unnecessary follow-up procedures, such as colposcopy or biopsy, and undue anxiety over the test results.
- False-negative. A false-negative test result means you really do have an HPV infection, but the test indicates that you don't. This might cause a delay in appropriate follow-up tests or procedures.
How you prepare
No special preparation is necessary before you have an HPV test. However, since an HPV test often is done at the same time as a Pap test, you can take these measures to make both tests as accurate as possible:
- Avoid intercourse, douching, or using any vaginal medicines or spermicidal foams, creams or jellies for two days before the test.
- Try not to schedule the test during your menstrual period. The test can be done, but your doctor can collect a better sample of cells at another time in your cycle.
What you can expect
An HPV test is usually done at the same time as a Pap test — a test that collects cells from your cervix to check for abnormalities or the presence of cancer. An HPV test can be done using the same sample from the Pap test or by collecting a second sample from the cervical canal.
During the procedure
Pap test
Pap test
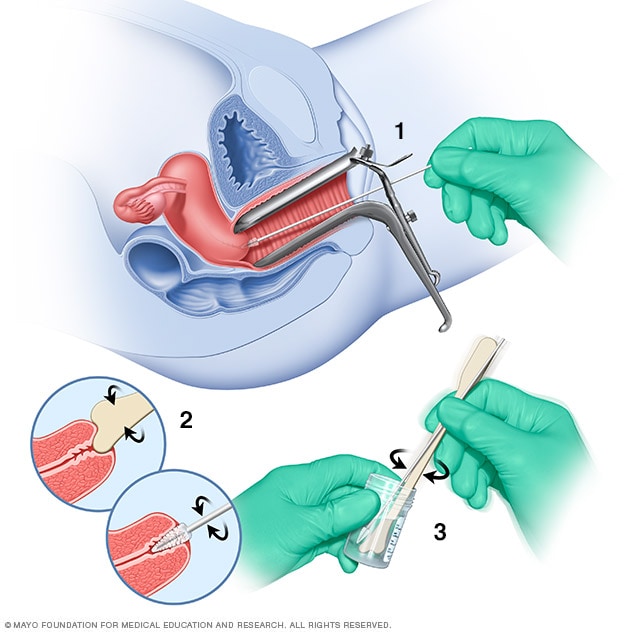
During a Pap test, a tool called a speculum holds the vaginal walls apart. A sample of cells from the cervix is collected using a soft brush and a flat scraping device called a spatula (1 and 2). The cells are placed in a bottle that contains a solution to preserve them (3). Or the cells may be smeared onto a glass slide. Later, the cells are checked under a microscope.
A combination Pap-HPV test is performed in your doctor's office and takes only a few minutes. You may be asked to undress completely or only from the waist down. You'll lie on your back on an exam table with your knees bent. Your heels rest in supports called stirrups.
Your doctor will gently insert an instrument called a speculum into your vagina. The speculum holds the vaginal walls apart so that your doctor can easily see your cervix. Inserting the speculum may cause a sensation of pressure in your pelvic area. Sometimes the speculum feels cold when it's first inserted.
Your doctor will then take samples of your cervical cells using a soft brush and a flat scraping device called a spatula. This doesn't hurt, and you may not even feel the sample being taken.
After the procedure
After your test, you can go about your normal daily activities without any restrictions. Ask your doctor about when you can expect to receive your test results.
Results
Results from your HPV test will come back as either positive or negative.
- Positive HPV test. A positive test result means that you have a type of high-risk HPV that's linked to cervical cancer. It doesn't mean that you have cervical cancer now, but it's a warning sign that cervical cancer could develop in the future. Your doctor will probably recommend a follow-up test in a year to see if the infection has cleared or to check for signs of cervical cancer.
- Negative HPV test. A negative test result means that you don't have any of the types of HPV that cause cervical cancer.
Depending on your test results, your doctor may recommend one of the following as a next step:
- Normal monitoring. If you're older than age 30, and your HPV test is negative and your Pap test is normal, you'll follow the generally recommended schedule for repeating both tests in five years.
- Colposcopy. In this follow-up procedure, which is recommended if your Pap test is abnormal, your doctor uses a special magnifying lens (colposcope) to more closely examine your cervix.
- Biopsy. In this procedure, usually done at the same time as colposcopy, your doctor takes a sample of cervical cells (biopsy) to be examined more closely under a microscope.
- Removal of abnormal cervical cells. To prevent abnormal cells from developing into cancerous cells, your doctor may suggest a procedure to remove the areas of tissue that contain the abnormal cells.
- Seeing a specialist. If your Pap test or HPV test results are abnormal, your doctor will probably refer you to a gynecologist for a colposcopic exam. If test results show that you might have cancer, you may be referred to a doctor who specializes in treating cancers of the female genital tract (gynecologic oncologist) for treatment.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Oct. 28, 2023