Overview
Endometrial ablation is a surgery that destroys the lining of the uterus. The lining of the uterus is called the endometrium. The goal of endometrial ablation is to reduce how much you bleed during periods, also called menstrual flow. In some people, menstrual flow may stop completely.
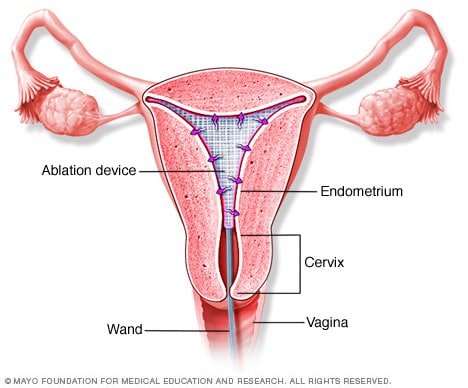
No cuts are needed for endometrial ablation. Your health care provider inserts slender tools through the vagina and into the natural opening of the uterus, also called the cervix.
The tools vary, depending on the method used to ablate the endometrium. Methods might include extreme cold, heated fluids, microwave energy or high-energy radiofrequencies.
Endometrial ablation can be done in your health care provider's office or in an operating room. The size and condition of your uterus, your health and other factors, such as the practice of your provider, can play a role in which endometrial ablation method you'll have.
Why it's done
Endometrial ablation is a treatment for very heavy menstrual blood loss. You might need an endometrial ablation if you have:
- Unusually heavy periods, sometimes defined as soaking a pad or tampon every two hours or less.
- Bleeding that lasts longer than eight days.
- A low red blood cell count from excessive blood loss. This is called anemia.
To reduce how much you bleed during periods, your health care provider might suggest birth control pills or an intrauterine device (IUD). Endometrial ablation is another option.
Endometrial ablation generally isn't recommended for women after menopause. It also isn't recommended for women who have:
- Certain uterus conditions.
- Cancer of the uterus, or an increased risk of cancer of the uterus.
- An active pelvic infection.
- A desire for future pregnancy.
Risks
Complications of endometrial ablation are rare and can include:
- Pain, bleeding or infection.
- Heat or cold damage to nearby organs.
- A puncture injury of the wall of the uterus from surgical tools.
Future fertility
You can still get pregnant after endometrial ablation. But the pregnancy is higher risk to you and the baby. The pregnancy might end in miscarriage because the lining of the uterus has been damaged. The placenta may not implant correctly, causing it to grow into the uterus wall. Or the pregnancy might occur in one of the fallopian tubes or cervix instead of the uterus. This is called an ectopic pregnancy.
If you have an endometrial ablation, long-lasting or permanent birth control is advised to prevent pregnancy.
How you prepare
In the weeks before the procedure, your health care provider typically will:
- Perform a pregnancy check. Endometrial ablation can't be done if you're pregnant.
- Check for cancer. A thin tube is inserted through the cervix to collect a small sample of the endometrium to be tested for cancer.
- Examine the uterus. Your provider may examine your uterus using an ultrasound. You also may have a procedure that uses a thin device with a light, called a scope, to look at the inside of your uterus. This is called hysteroscopy. These tests can help your provider choose which endometrial ablation procedure to use.
- Remove an IUD. Endometrial ablation isn't done with an IUD in place.
- Thin your endometrium. Some types of endometrial ablation work better when the uterine lining is thin. Your health care provider might have you take medicine to thin the lining. Another option is to do a dilation and curettage (D&C). In this procedure, your provider uses a special tool to remove extra tissue from the lining of the uterus.
- Talk about anesthesia options. Ablation often can be done with sedation and pain medicine. This may include numbing shots into the cervix and uterus. But, sometimes general anesthesia is used. This means you're in a sleep-like state during the procedure.
What you can expect
During the procedure
Radiofrequency ablation
Radiofrequency ablation
During radiofrequency ablation, a triangular ablation device uses radiofrequency energy to destroy the tissue lining the uterus. The lining is called the endometrium. The ablation device is then removed from the uterus.
Endometrial ablation may be done in your provider's office or in an operating room.
The opening in your cervix may be made wider through a process called dilation. This allows room for the tools needed for the ablation to be inserted. Dilation of the cervix can happen with medicine or by inserting a series of rods that gradually get bigger.
Endometrial ablation procedures vary by the method used to remove or destroy the endometrium. Options include:
- Cryotherapy ablation. A probe is inserted inside the uterus and cooled. Extreme cold at the tip of the probe freezes the lining of the uterus in sections, destroying the uterine lining. Ultrasound allows your provider to track the progress. Each freeze cycle takes about six minutes. The number of cycles needed depends on the size and shape of the uterus.
- Hydrothermal ablation. Fluid is inserted into the uterus and heated for about 10 minutes. The heat destroys the uterine lining. An advantage of this method is that it can be performed in someone who has an irregular-shaped uterus from altered tissue growth. Misshaping of the uterus can occur from conditions such as lesions inside the uterus or uterine fibroids.
- Radiofrequency ablation. A special instrument opens a flexible, triangular device inside the uterus. The ablation device sends out radiofrequency energy that destroys the uterine lining in 1 to 2 minutes. The device is then removed from the uterus.
- Electrocautery ablation. A slender scope is used to see inside the uterus. A tool, such as a wire loop or a probe with a rollerball tip or an electrode tip, is passed through the scope. The tool uses electric current to remove or destroy the uterine lining. Electrocautery ablation requires general anesthesia. This method of ablation is used less often than other options.
- Microwave ablation. A device is inserted into the uterus. The device applies microwave energy to the uterine lining and destroys it. New devices using this method of ablation are in development.
After the procedure
After endometrial ablation, you might have:
- Cramps. You may have period-like cramps for a few days. Nonprescription pain-relief medicine such as ibuprofen (Advil, Motrin IB, others) or acetaminophen (Tylenol, others) can help relieve cramping.
- Vaginal discharge. A watery discharge, mixed with blood, may occur for a few weeks. The discharge is typically heaviest for the first few days after the procedure.
- Frequent urination. You may need to pass urine more often during the first 24 hours after endometrial ablation.
Ask your health care provider about when you can return to your usual activities, such as exercise, work and sex. During a follow-up visit, your provider can check your healing.
Results
It might take a few months to see the final results. But endometrial ablation often reduces the amount of blood lost during periods. You may have lighter periods. Or you may stop having periods entirely.
Endometrial ablation isn't a sterilization procedure. You should continue to use birth control. Pregnancy might still be possible, but it will likely be dangerous to you and the baby. It may end in miscarriage. Permanent sterilization is also an option to avoid pregnancy after the procedure.
Dec. 20, 2022