Overview
Electrocardiogram
Electrocardiogram
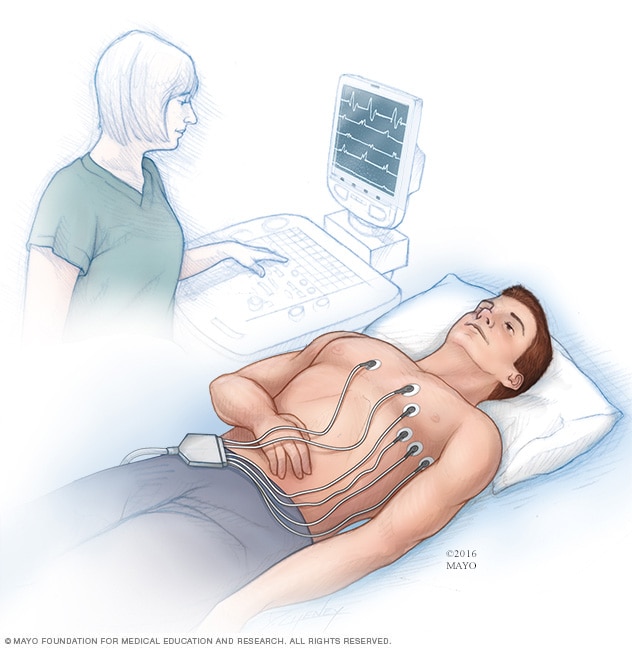
An electrocardiogram (ECG or EKG) is a test to record the electrical signals in the heart. It shows how the heart is beating. Sticky patches called electrodes are placed on the chest and sometimes on the arms or legs. Wires connect the patches to a computer, which prints or displays results.
An electrocardiogram (ECG or EKG) is a quick test to check the heartbeat. It records the electrical signals in the heart. Test results can help diagnose heart attacks and irregular heartbeats, called arrhythmias.
ECG machines can be found in medical offices, hospitals, operating rooms and ambulances. Some personal devices, such as smartwatches, can do simple ECGs. Ask your healthcare professional if this is an option for you.
Products & Services
Types
Why it's done
An electrocardiogram (ECG or EKG) is done to check the heartbeat. It shows how fast or how slow the heart is beating. ECG test results can help your care team diagnose:
- Irregular heartbeats, called arrhythmias.
- A previous heart attack.
- The cause of chest pain. For example, it may show signs of blocked or narrowed heart arteries.
An ECG also may be done to learn how well a pacemaker and heart disease treatments are working.
You may need an ECG if you have:
- Chest pain.
- Dizziness, lightheadedness or confusion.
- Pounding, skipping or fluttering heartbeat.
- Fast pulse.
- Shortness of breath.
- Weakness or fatigue.
- Reduced ability to exercise.
If you have a family history of heart disease, you may need an electrocardiogram to screen for heart disease, even if you don't have symptoms. The American Heart Association says ECG screening may be considered for those at low risk of heart disease in general, even if there are no symptoms. Most heart doctors consider an ECG as a basic tool to screen for heart disease, although its use needs to be individualized.
If symptoms tend to come and go, a regular ECG may not find a change in the heartbeat. Your healthcare team may suggest wearing an ECG monitor at home. There are several types of portable ECGs.
- Holter monitor. This small, portable ECG device is worn for a day or more to record the heart's activity. You wear it at home and during daily activities.
- Event monitor. This device is like a Holter monitor, but it records only at certain times for a few minutes at a time. It's typically worn for about 30 days. You usually push a button when you feel symptoms. Some devices automatically record when an irregular heart rhythm occurs.
Some personal devices, such as smartwatches, have electrocardiogram apps. Ask your care team if this is an option for you.
 ECG on medical helicopter
ECG on medical helicopter
A person receives an ECG while on a helicopter for medical transport.
More Information
Risks
There is no risk of electric shock during an electrocardiogram. The sensors, called electrodes, do not make electricity.
Some people may get a slight rash where the patches were placed. Removing the patches may feel uncomfortable for some people. It's similar to taking off a bandage.
How you prepare
You don't need to do anything to prepare for an electrocardiogram (ECG or EKG). Tell your healthcare team about all the medicines you take, including those bought without a prescription. Some medicines and supplements may affect the test results.
What you can expect
An electrocardiogram (ECG or EKG) can be done in a medical office or hospital. The test also may be done in an ambulance or other emergency vehicle.
Before
Before getting an electrocardiogram, you may be asked to change into a hospital gown. A member of your healthcare team may shave any hair on the area where the electrode patches are placed. This helps the patches better stick to the skin.
Once you're ready, you usually lie down on an examining table or bed.
During
During an electrocardiogram, up to 12 sticky patches called electrodes are attached to the chest and sometimes to the arms or legs. Wires connect the patches to a computer. The computer prints or displays results. Results are shown in waves. The waves are the signals that travel through the heart with each heartbeat.
You can breathe during the test. But stay still and do not talk. Movement may interfere with the test results.
After
Unless you're having a heart problem that needs immediate treatment, you can usually return to your daily activities after having an electrocardiogram.
Results
Your healthcare professional might talk to you about the electrocardiogram (ECG or EKG) results the same day as the test. Sometimes the results are shared with you at your next appointment.
A healthcare professional looks for heart signal patterns in the electrocardiogram results. Doing this gives information about the heart's health such as:
- Heart rate. The heart rate is the number of times the heart beats a minute. You can measure your heart rate by checking your pulse. But an ECG may be helpful if your pulse is difficult to feel or too irregular to count accurately. ECG results can help diagnose an unusually fast heart rate, called tachycardia, or an unusually slow heart rate, called bradycardia.
- Heart rhythm. The heart's rhythm is the time between each heartbeat. It's also the signal pattern between each beat. An ECG can show irregular heartbeats, called arrhythmias. Examples include atrial fibrillation (AFib) and atrial flutter.
- Heart attack. An ECG can diagnose a current or previous heart attack. The patterns on the ECG results can help a healthcare professional learn which part of the heart is damaged.
- Blood and oxygen supply to the heart. An ECG done while you're having chest pain symptoms can help your care team learn whether reduced blood flow to the heart is the cause.
- Heart structure changes. ECG results can provide clues about an enlarged heart, congenital heart defects and other heart conditions.
If results show a change in the heartbeat, you may need more testing. For example, you might have an ultrasound of the heart, called an echocardiogram.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.