Overview
Breast reconstruction is a surgical procedure that restores shape to your breast after mastectomy — surgery that removes your breast to treat or prevent breast cancer.
One type of breast reconstruction uses breast implants — silicone devices filled with silicone gel or salt water (saline) — to reshape your breasts. Breast reconstruction with breast implants is a complex procedure performed by a plastic surgeon.
The breast reconstruction process can start at the time of your mastectomy (immediate reconstruction), or it can be done later (delayed reconstruction). The breast reconstruction process usually requires two or more operations. You can also expect to several appointments over two to three months after your initial surgery in order to expand and stretch the skin on your chest in preparation for the implant.
Breast reconstruction won't re-create the exact look and feel of your natural breast. However, the contour of your new breast may restore a silhouette similar to what you had before mastectomy.
Risks
Breast reconstruction with a breast implant carries the possibility of complications, including:
- Breasts that don't match each other in size or appearance (asymmetry)
- Breast pain
- Implant rupture or deflation
- Poor healing of incisions
- Increased risk of future breast surgery to replace or remove the breast implant
- Changes in breast sensation
- Infection
- Bleeding
- Scar tissue that forms and compresses the implant and breast tissue into a hard, unnatural shape (capsular contracture)
- Risks associated with anesthesia
- Very low, but increased risk of a rare immune system cancer called anaplastic large cell lymphoma (ALCL) that's associated with textured breast implants, though more research is needed to understand the relationship between ALCL and breast implants
Correcting any of these complications may require additional surgery.
If you need adjuvant radiation therapy to the skin and chest wall after a mastectomy (post-mastectomy radiation), you might not be an ideal candidate for breast implant reconstruction. Having a breast implant may make it more difficult to deliver the radiation therapy effectively, and the implant may need to be deflated. There may also be a higher risk of complications. The skin and underlying tissue may become firmer, discolored and swollen due to radiation therapy.
How you prepare
Before a mastectomy, your doctor may recommend that you meet with a plastic surgeon. Consult a plastic surgeon who's board certified and experienced in breast reconstruction following mastectomy. Ideally, your breast surgeon and the plastic surgeon should work together to develop the best surgical treatment and breast reconstruction strategy in your situation.
Your plastic surgeon will describe your surgical options and discuss the advantages and disadvantages of implant-based reconstruction, and may show you photos of women who have had different types of breast reconstruction. Your body type, health status and cancer treatment factor into which type of reconstruction will provide the best result. The plastic surgeon provides information on the anesthesia, the location of the operation and what kind of follow-up procedures may be necessary.
Your plastic surgeon may discuss the pros and cons of surgery on your opposite breast, even if it's healthy, so that it more closely matches the shape and size of your reconstructed breast. Surgery to remove your healthy breast (contralateral prophylactic mastectomy) can double the risk of surgical complications, such as bleeding and infection. Also, there may be less satisfaction with cosmetic outcomes after surgery.
Before your surgery, follow your doctor's specific instructions on preparing for the procedure. This may include guidelines on eating and drinking, adjusting current medications, and quitting smoking.
What you can expect
Tissue expansion
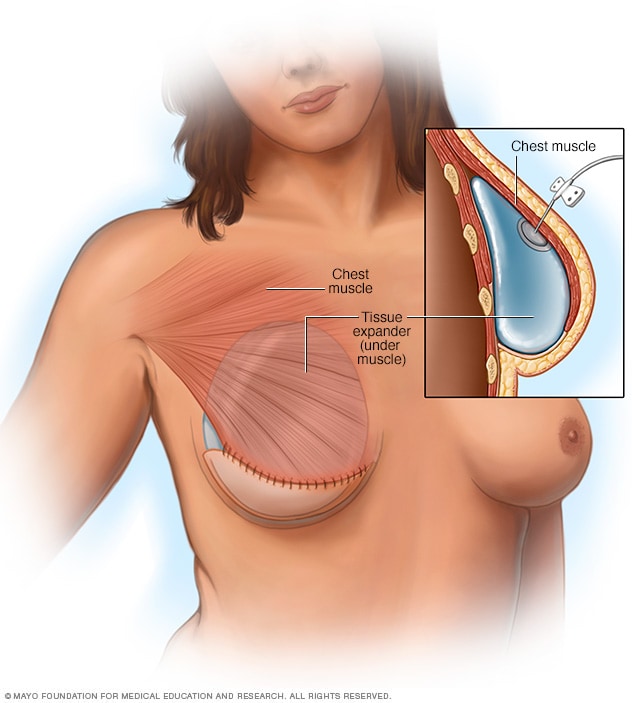
Tissue expansion
During tissue expansion, a balloon inserted under your chest muscle is gradually filled with saline over a period of several weeks or months. The gradual inflation of the balloon stretches the skin and tissue over your chest to make room for an implant.
Breast reconstruction begins with placement of a breast implant or tissue expander, either at the time of your mastectomy (immediate reconstruction) or during a later procedure (delayed reconstruction). Breast reconstruction often requires multiple operations, even if you choose immediate reconstruction.
Breast implants
A breast implant is a round or teardrop-shaped silicone shell filled with salt water (saline) or silicone gel. Once restricted because of safety concerns, silicone gel implants are now considered safe.
A plastic surgeon places the implant either behind or in front of the muscle in your chest (pectoral muscle). Implants that are put in front of the muscle are held in place using a special tissue called acellular dermal matrix. Over time, your body replaces this tissue with collagen.
Some women are able to have the permanent breast implant placed at the time of the mastectomy (direct-to-implant reconstruction). However, many women require a two-stage process, using a tissue expander before the permanent implant is placed.
Tissue expanders
Pre-pectoral breast implant
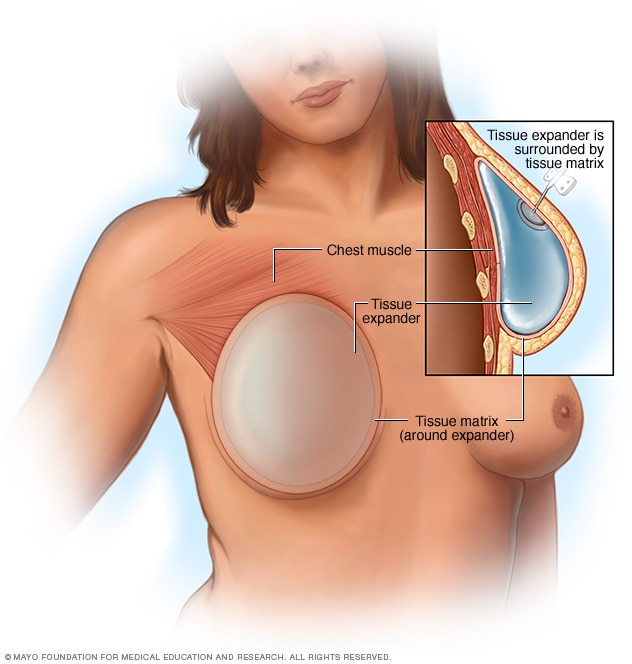
Pre-pectoral breast implant
A breast implant that's placed on top of the chest muscle is called a pre-pectoral breast implant. It's often done in two operations. First, a surgeon places a tissue expander under the skin. The tissue expander is a temporary breast implant. It works like a balloon. The size can be adjusted to the size you prefer. In a second operation, a surgeon removes the expander and replaces it with a breast implant.
Tissue expansion is a process that stretches your remaining chest skin and soft tissues to make room for the breast implant. Your surgeon places a balloonlike tissue expander under or over your pectoral muscle at the time of your mastectomy. Over the next few months, through a small valve under your skin, your doctor or nurse uses a needle to inject saline into the valve, filling the balloon in stages.
This gradual process allows the skin to stretch over time. You'll go to your doctor every week or two to have the saline injected. You may experience some discomfort or pressure as the implant expands.
A newer type of tissue expander uses carbon dioxide. This remote-controlled expander releases the gas from an internal reservoir. Compared with the expansion using saline, the gradual expansion using carbon dioxide may decrease the amount of discomfort you feel.
After the tissue is adequately expanded, your surgeon performs a second surgery to remove the tissue expander and replace it with a permanent implant, which is placed in the same place as the tissue expander.
Recovery
You may be tired and sore for several weeks after surgery. Your doctor will prescribe medication to help control your pain.
Getting back to normal activities may take six weeks or longer. Take it easy during this period.
Your doctor will let you know of restrictions to your activities, such as avoiding overhead lifting or strenuous physical activities. Don't be surprised if it seems to take a long time to bounce back from surgery — it may take as long as a year or two to feel completely healed.
Generally, you'll follow up with your plastic surgeon on a yearly basis to monitor your reconstructed breast after the reconstruction is complete. Make an appointment sooner than that, however, if you have any concerns about your reconstruction.
Nipple reconstruction
Nipple reconstruction
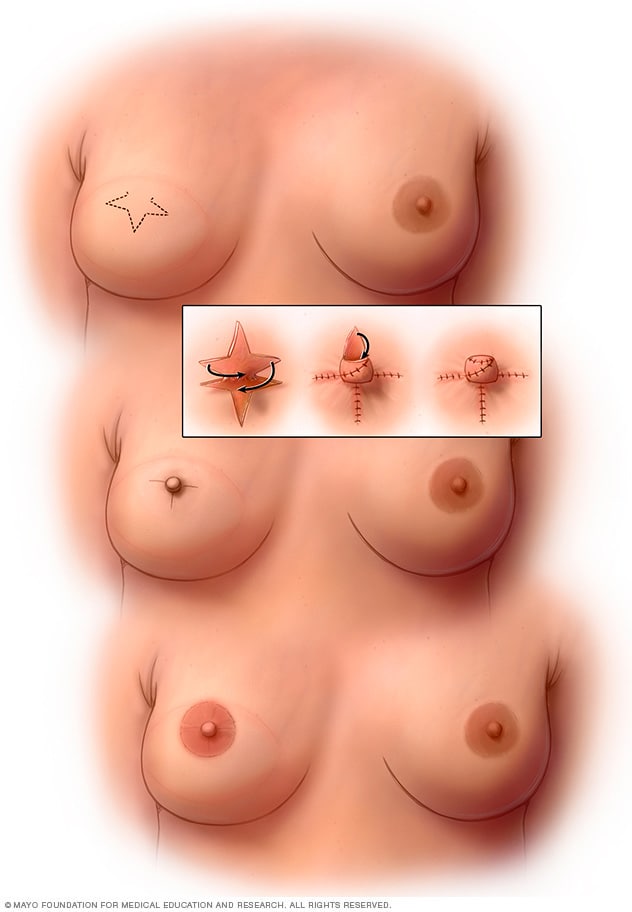
Nipple reconstruction
After your breast has healed from reconstruction or mastectomy, a plastic surgeon can reconstruct a new nipple and areola. The surgeon makes a star-shaped incision to form the new nipple and then adds a tattoo to shade in the new areola.
Breast reconstruction may also entail reconstruction of your nipple, if you choose, including tattooing to define the dark area of skin surrounding your nipple (areola).
Future breast cancer screening
If you've had only one breast reconstructed, you'll need to have screening mammography done regularly on your other breast. Mammography isn't necessary on breasts that have been reconstructed.
You may opt to perform breast self-exams on your natural breast and the skin and surrounding area of your reconstructed breast. This may help you become familiar with the changes to your breast after surgery so that you can be alert to any new changes and report those to your doctor.
Results
Keep your expectations realistic when anticipating the outcome of your surgery. Breast reconstruction surgery offers many benefits, but it won't make you look or feel exactly like you did before your mastectomy.
What breast reconstruction can do:
- Give you a breast contour
- Provide improved symmetry to your breasts so that they look similar under clothing or a bathing suit
- Help you avoid the need for a form (external prosthesis) inside your bra
What breast reconstruction may do:
- Improve your self-esteem and body image
- Partially erase the physical reminders of your disease
- Require additional surgery to correct reconstructive problems
What breast reconstruction won't do:
- Make you look exactly the same as before
- Give your reconstructed breast the same sensations as your normal breast
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
The Mayo Clinic experience and patient stories
Our patients tell us that the quality of their interactions, our attention to detail and the efficiency of their visits mean health care like they've never experienced. See the stories of satisfied Mayo Clinic patients.
Dec. 28, 2022