Sept. 01, 2015
Lipodystrophies are a heterogeneous group of rare acquired and inherited disorders characterized by selective loss of adipose tissue. Vinaya Simha, MBBS, M.D., an endocrinology consultant at Mayo Clinic's campus in Rochester, Minnesota, says: "While the first reported case of lipodystrophy dates back to the late 19th century, much progress has occurred in the past decade in understanding both the molecular mechanisms of fat loss and its optimal treatment.
"These advances have not only offered a new ray of hope for patients with these rare syndromes but have also provided valuable insight into our understanding of adipose tissue biology, and the pathophysiology of other common obesity-related metabolic disorders such as diabetes, dyslipidemia, insulin resistance and steatohepatitis."
Classification and clinical feature
Lipodystrophy syndromes
Lipodystrophy syndromes
Classification and overview of different lipodystrophy syndromes
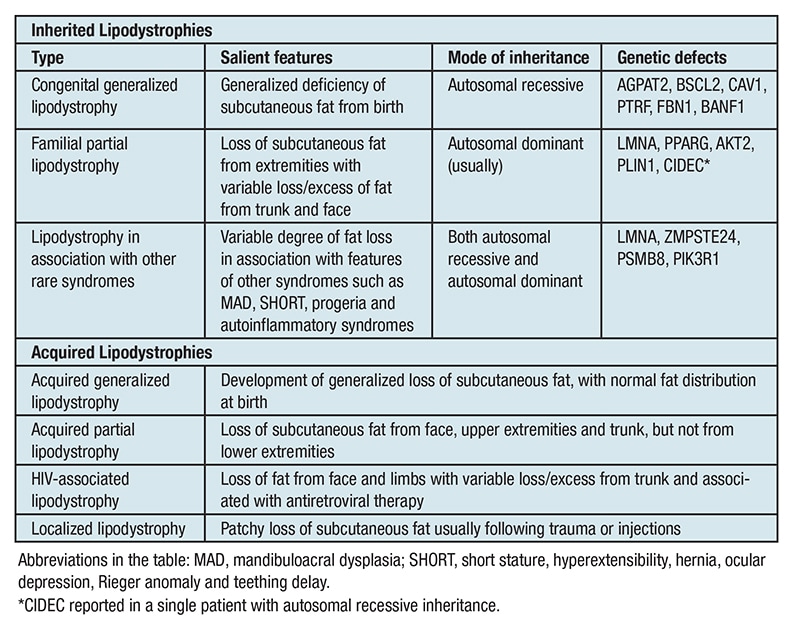
Dr. Simha explains: "Loss of adipose tissue can occur either due to genetic or acquired causes, and can involve either the entire body or be restricted to certain areas like the extremities, often with excess fat deposition in the unaffected areas. Accordingly, both acquired and genetic lipodystrophy may be associated with either a generalized or a partial lipodystrophy phenotype. The table provides a brief summary of the genotypic and phenotypic diversity of the different lipodystrophy syndromes."
Congenital generalized lipodystrophy (CGL) is one of the most well-studied lipodystrophy syndromes with over 300 reported cases in the literature. Affected subjects have extreme paucity of adipose tissue from birth, leading to a muscular appearance with prominent veins and an acromegaloid appearance, along with severe acanthosis nigricans, hepatosplenomegaly, and early onset of diabetes, hypertriglyceridemia and steatohepatitis. Marked hypoleptinemia is a universal feature of this disease.
Patients with familial partial lipodystrophy (FPL) have normal fat distribution at birth but usually develop fat loss from the extremities after puberty. The most well-studied type of FPL is the Dunnigan variety (FPLD) in which fat loss from the limbs and often the trunk, especially anteriorly and over the breasts, is usually accompanied by excess fat deposition over the face and neck. Metabolic abnormalities are similar to those seen in patients with CGL but may not be as severe in some patients. Since the extent of fat loss is not uniform, circulating leptin levels may also vary from low to normal in these patients.
Acquired lipodystrophies may occur in association with other autoimmune disorders or panniculitis, or may be idiopathic. Patients with acquired generalized lipodystrophy (AGL) may show severe metabolic complications similar to patients with CGL, while patients with acquired partial lipodystrophy (APL), also known as Barraquer-Simons syndrome, who invariably have well-preserved lower body fat, have lesser incidences of metabolic complications compared with other lipodystrophy syndromes. Rare forms of acquired partial lipodystrophy associated with autoinflammatory syndromes may however be associated with significant metabolic abnormalities.
The most prevalent form of lipodystrophy is seen in association with HIV infection (LD-HIV), with 40 to 50 percent of patients on long-term antiretroviral therapy being affected by either generalized lipoatrophy or partial fat loss involving the face and extremities. Even though the newer protease inhibitors cause less impact on body fat distribution and lipid homeostasis, LD-HIV is emerging as one of the most important challenges for long-term care of patients with HIV infection.
Novel treatment options for the metabolic complications of lipodystrophy
Dr. Simha notes: "Despite the marked heterogeneity in etiology and clinical features of the different lipodystrophy syndromes, they share common metabolic abnormalities such as diabetes with marked insulin resistance, severe hypertriglyceridemia, steatohepatitis and features of polycystic ovary syndrome.
"Often, the severity of these metabolic disturbances is related to the extent of fat loss, thus indicating the critical role of adipose tissue in maintenance of normal glucose and lipid homeostasis, and not surprisingly, adipose tissue transplantation in lipodystrophic mice has been shown to ameliorate hyperglycemia, hyperlipidemia and hepatic steatosis.
"However, if the donor fat was obtained from leptin knockout mice whose adipocytes could not secrete leptin, no metabolic benefits were observed, thus highlighting the endocrine functions of adipose tissue in preventing metabolic complications. These observations have led to the development of leptin-replacement therapy in patients with generalized lipodystrophy."
In the initial open-label, prospective, phase II study, nine female patients with severe hypoleptinemia and metabolic abnormalities were treated with recombinant human leptin for four months. Results of the study by Elif A. Oral, M.D., and others were published in the New England Journal of Medicine in 2002.
Dr. Simha, one of the co-authors of the study, explains: "Marked improvements in multiple metabolic variables were noted including a nearly 2 point reduction in hemoglobin A1C, a 60 percent reduction in serum triglycerides and hepatic transaminases, and 28 percent reduction in liver volume, besides improvements in glucose tolerance and insulin sensitivity. Further, leptin therapy facilitated a significant reduction in the burden of pharmacotherapy, and it was possible to reduce or completely stop glucose- and lipid-lowering medications in most of the subjects.
"Longitudinal follow-up of these patients for up to five years has demonstrated the durability of leptin's beneficial effects, and other recent studies, including a study published in Diabetes in 2005 that discusses beneficial effects in children, have also shown similar results.
"A significant finding across many of these studies is a marked reduction in hepatic fat and histologic improvement in steatohepatitis. Based on these studies, as reviewed in Expert Review of Endocrinology & Metabolism in 2014, the Food and Drug Administration has approved recombinant human leptin (available as metreleptin) for treatment of adult and pediatric patients with generalized lipodystrophy. It is administered as a daily subcutaneous injection after reconstitution, and is likely to improve metabolic variables, which are usually very resistant to traditional therapies."
Leptin therapy for lipodystrophy: Unresolved questions
Dr. Simha summarizes: "Leptin-replacement therapy is doubtless a promising option for patients with lipodystrophy, but many questions remain unanswered. One of them is the role of leptin therapy in patients with partial lipodystrophy who have variable fat loss and leptin levels.
"Despite a recent study in 24 female subjects with FPLD, published the Journal of Clinical Endocrinology & Metabolism in 2012, which showed a similar reduction in serum and hepatic triglycerides in those with severe and moderate hypoleptinemia, the overall response to leptin therapy in patients with partial lipodystrophy is not as robust as in those with generalized lipodystrophy. Indeed, leptin therapy is not approved for patients with partial lipodystrophy, including those with LD-HIV. The 'anti-steatotic' effect of leptin in patients with partial lipodystrophy without hypoleptinemia needs to be studied.
"The long-term efficacy and safety of leptin therapy also need to be closely examined, as neutralizing antibodies may influence the biological activity of both endogenous and exogenous leptin. Jacques Beltrand, M.D., and others discussed immunological origin of resistance to leptin-replacement therapy in Berardinelli-Seip congenital lipodystrophy in European Journal of Endocrinology in 2010. Rare cases of hematologic malignancies also have been noted during leptin-replacement therapy in patients with AGL.
"Further, the molecular mechanisms underlying insulin resistance in lipodystrophy and its amelioration by leptin therapy need to be elucidated. We are specifically trying to study protein turnover and insulin action in the hypertrophied skeletal muscles of patients with lipodystrophy to get a better understanding of the interplay between adipose tissue and skeletal muscle in maintaining glucose and lipid homeostasis. These are indeed exciting times for both patients with lipodystrophy, and physicians and investigators involved in their care."
For more information
Oral EA, et al. Leptin-replacement therapy for lipodystrophy. New England Journal of Medicine. 2002;346:570.
Javor ED, et al. Long-term efficacy of leptin replacement in patients with generalized lipodystrophy. Diabetes. 2005;54:1994.
Simha V. Metreleptin for metabolic disorders associated with generalized or partial lipodystrophy. Expert Review of Endocrinology & Metabolism. 2014;9:205.
Simha V, et al. Comparison of efficacy and safety of leptin replacement therapy in moderately and severely hypoleptinemic patients with familial partial lipodystrophy of the Dunnigan variety. Journal of Clinical Endocrinology & Metabolism. 2012;97:785.
Beltrand J, et al. Resistance to leptin-replacement therapy in Berardinelli-Seip congenital lipodystrophy: An immunological origin. European Journal of Endocrinology. 2010;162:1083.