April 21, 2018
A 51-year-old woman was referred to Mayo Clinic for evaluation of persistent hypercalcemia after parathyroid surgery. She was diagnosed with primary hyperparathyroidism at an outside institution one year prior with appropriate laboratory work-up, including elevated 24-hour urine calcium excretion, and deemed a suitable candidate for surgery given persistent fatigue and osteopenia documented with bone mineral density testing.
Preoperative imaging, including neck ultrasound and a parathyroid sestamibi scan, failed to localize abnormal parathyroid tissue. She subsequently underwent bilateral neck exploration with left superior, left inferior and right inferior parathyroidectomy as well as right superior parathyroidectomy with auto-transplantation into the left neck infrahyoid muscles.
The patient's serum parathyroid hormone (PTH) levels were persistently elevated intraoperatively and, unfortunately, she continued to have biochemical primary hyperparathyroidism postoperatively. Additional imaging included a neck ultrasound, parathyroid sestamibi scan and 4-D computerized tomography (CT) neck scan — all of these imaging modalities failed to localize a parathyroid adenoma.
The patient's past medical history was significant for depression and primary hypothyroidism. There was no family history of hypercalcemia or parathyroid surgery. Relevant medications included cholecalciferol 10,000 IU once daily.
Patient's laboratory evaluation
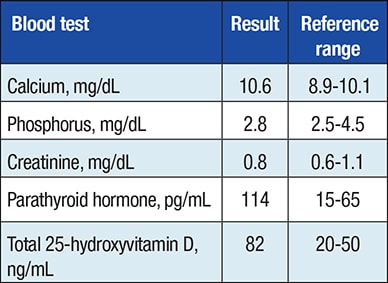
Patient's laboratory evaluation
Laboratory values obtained after the first operation, but before the second operation.
Her laboratory evaluation at Mayo Clinic was consistent with persistent primary hyperparathyroidism. Parathyroid sestamibi imaging with single-photon emission computerized tomography (SPECT) showed ectopic sestamibi uptake in the lower right midchest without discordance in the neck on planar images.
SPECT images confirmed an approximately 1-cm soft tissue nodule in the right paracardiac fat superiorly and just anterior and to the right of the lower superior vena cava and above the right atrial junction, consistent with a solitary parathyroid gland in the anterior mediastinum.
Axial and coronal images from SPECT scan
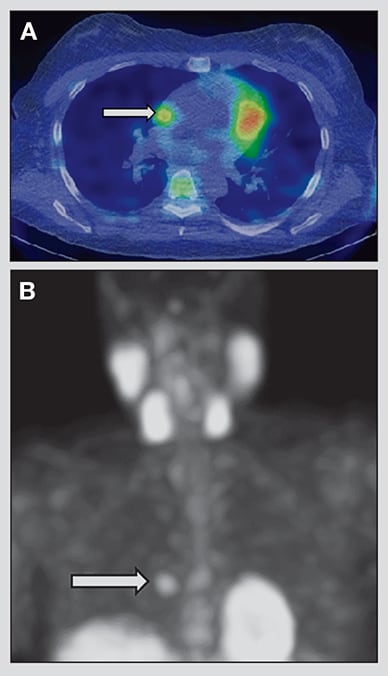
Axial and coronal images from SPECT scan
Axial (A) and coronal (B) images from parathyroid sestamibi SPECT scan demonstrating right paracardiac soft tissue nodule with intense sestamibi uptake (arrows).
Arterial phase MRI of the chest
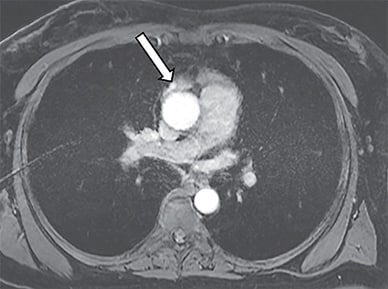
Arterial phase MRI of the chest
Arterial phase magnetic resonance imaging of the chest confirmed an enhancing 7-mm nodule (arrow) in the right lobe of the residual thymus in the anterior mediastinum.
Arterial phase magnetic resonance imaging of the chest confirmed an enhancing 7-mm nodule in the right lobe of the residual thymus in the anterior mediastinum, corresponding to the focal sestamibi uptake on SPECT imaging.
Endocrine and Thoracic Surgery collaborated to perform a partial thymectomy and resection of intrathymic ectopic parathyroid gland through right thoracoscopy and parathyroid auto-transplantation to the right superior chest wall. Intraoperative serum PTH concentrations dropped to less than 6 pg/mL. Surgical pathology revealed an intrathymic parathyroid adenoma (30 mg) with hypercellular parathyroid tissue.
The patient recovered well and had a resolution of her hypercalcemia postoperatively.
Persistent hyperparathyroidism after parathyroid surgery is most likely due to a missed parathyroid adenoma. The thymus has been reported as the most common ectopic site for parathyroid adenomas, followed by the thyroid gland, undescended glands, carotid sheath and the retroesophageal space.
Most supernumerary parathyroid glands are within the thymus. In the re-operative setting in particular, surgery can be challenging due to anatomical variability, limited localization studies and the possibility of supernumerary glands; therefore, a good understanding of the anatomy and embryology of the parathyroid glands is important to minimize the risk of permanent hypoparathyroidism.
Accurate localizing imaging studies including a neck ultrasound, parathyroid sestamibi scan and magnetic resonance imagining (MRI) are essential. In this patient, the imaging studies performed before the patient's first surgery failed to show the culprit lesion because the region of interest scanned did not extend inferiorly enough to sufficiently assess the mediastinum. Parathyroid sestamibi imaging with SPECT can improve the sensitivity in localizing parathyroid adenomas and increase diagnostic confidence.
Intraoperative ultrasound and PTH sampling are important to ensure that the culprit lesion has been successfully resected.
Key message
Ectopic parathyroid tissue should be considered in patients with persistent primary hyperparathyroidism, and when this occurs, surgical management is best undertaken by a multidisciplinary team.