Overview
Tachycardia heartbeat
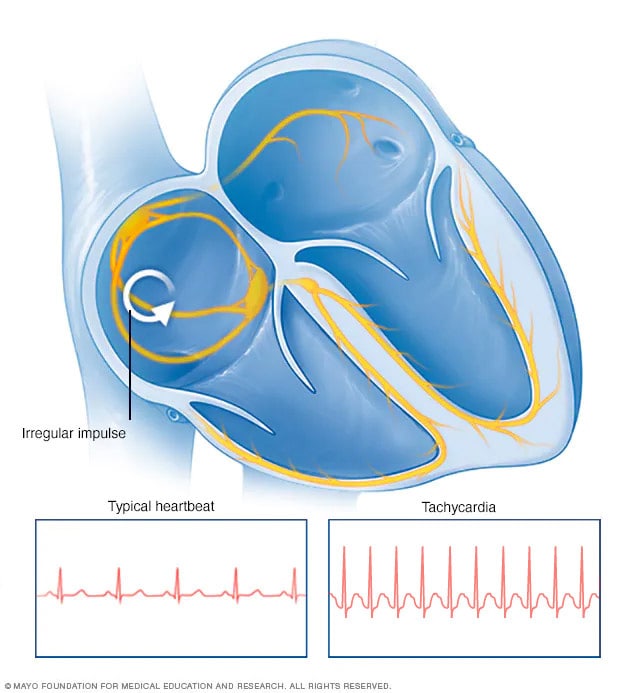
Tachycardia heartbeat
In tachycardia, an irregular electrical signal, called an impulse, starts in the upper or lower chambers of the heart. This causes the heart to beat faster.
Tachycardia (tak-ih-KAHR-dee-uh) is the medical term for a heart rate over 100 beats a minute. Many types of irregular heart rhythms, called arrhythmias, can cause tachycardia.
A fast heart rate isn't always a concern. For instance, the heart rate usually rises during exercise or as a response to stress.
Tachycardia may not cause any symptoms or complications. But sometimes it's a warning of a medical condition that needs attention. Some forms of tachycardia can lead to serious health problems if left untreated. Such problems may include heart failure, stroke or sudden cardiac death.
Treatment for tachycardia may include specific actions or movements, medicine, cardioversion, or surgery to control a rapid heartbeat.
Types
There are many different types of tachycardia. Sinus tachycardia refers to a usual increase in the heart rate often caused by exercise or stress.
Other types of tachycardia are grouped according to cause and the part of the heart causing the fast heart rate. Common types of tachycardia caused by irregular heart rhythms include:
- Atrial fibrillation, also called AFib. This is the most common type of tachycardia. Chaotic, irregular electrical signals start in the upper chambers of the heart, called the atria. These signals trigger a fast heartbeat. A-fib may be temporary. But some episodes won't end unless treated.
- Atrial flutter. Atrial flutter is similar to A-fib, but heartbeats are more organized. Episodes of atrial flutter may go away by themselves or may need treatment. People who have atrial flutter also often have A-fib at other times.
- Ventricular tachycardia. This irregular heart rhythm starts in the lower heart chambers, called the ventricles. The fast heart rate doesn't let the ventricles fill and squeeze to pump enough blood to the body. Episodes may be brief and last only a couple of seconds without causing harm. But episodes lasting more than a few seconds can be life-threatening.
- Supraventricular tachycardia (SVT). Supraventricular tachycardia is a broad term that includes irregular heart rhythms that start above the lower heart chambers. Supraventricular tachycardia causes episodes of a pounding heartbeat that begin and end abruptly.
- Ventricular fibrillation. This serious condition can be deadly if the heart rhythm isn't reset within minutes. Rapid, chaotic electrical signals cause the lower heart chambers to quiver instead of squeezing in a coordinated way. Most people with this type of irregular heart rhythm have heart disease or have had a serious injury, such as being struck by lightning.
Mayo Clinic Minute: Identifying and treating atrial fibrillation
Mayo Clinic electrophysiologist Fred Kusumoto, M.D., explains what happens in the heart to create atrial fibrillation and what can be done to fix it.
Jeff Olsen: This is a normal heartbeat. [HEART BEATING] Atrial fibrillation interrupts this regular beat.
Fred Kusumoto, M.D., Cardiology, Mayo Clinic: In atrial fibrillation, instead of the atria squeezing in a normal regular fashion, the atria beat irregularly and chaotically.
Jeff Olsen: Dr. Fred Kusumoto is an electrophysiologist at Mayo Clinic.
Dr. Kusumoto: In some cases people feel their heart palpitating or beating very, very fast or a flip-flop in their heart or chest area. Other times, people just notice that they're more short of breath when they walk upstairs.
Jeff Olsen: Dr. Kusumoto says atrial fibrillation decreases the heart's blood pumping efficiency and puts a patient at higher risk for blood clots, heart failure, and stroke. In some cases, atrial fibrillation can be corrected with medication or by administering a shock to a sedated patient's heart. In other instances, a procedure called catheter ablation may be used to scar tissue that's creating the erratic signals [HEART BEATING] in the hopes of getting back to that normal beat.
Symptoms
Some people with tachycardia have no symptoms. The fast heartbeat may be discovered when a physical exam or heart tests are done for another reason.
In general, tachycardia may cause these symptoms:
- Racing, pounding heartbeat or flopping in the chest, called palpitations.
- Chest pain.
- Fainting.
- Lightheadedness.
- Rapid pulse.
- Shortness of breath.
When to see a doctor
Many things can cause tachycardia. If you feel like your heart is beating too fast, make an appointment for a health checkup.
Seek immediate medical help if you have:
- Chest pain or discomfort.
- Shortness of breath.
- Weakness.
- Dizziness or lightheadedness.
- Fainting or near fainting.
A type of tachycardia called ventricular fibrillation is an emergency that requires immediate medical attention.
During ventricular fibrillation, blood pressure drops dramatically. The person's breathing and pulse stop because the heart is not pumping any blood to the body. This also is called cardiac arrest. The person usually falls down, also called collapses.
If this happens, do the following:
- Call 911 or the emergency number in your area.
- Start CPR. CPR helps keep blood flowing to the organs until other treatments can start.
- If you're not trained in CPR or worried about giving rescue breaths, then provide hands-only CPR. Push hard and fast on the center of the chest at a rate of 100 to 120 compressions a minute until paramedics arrive. The American Heart Association suggests doing compressions to the beat of the song "Stayin' Alive." You don't need to do rescue breathing.
- Have someone get an automated external defibrillator (AED) if one is nearby. An AED is a portable device that delivers a shock to reset the heart rhythm. No training is needed to use the device. The AED tells you what to do. It's programmed to give a shock only when appropriate.
Causes
Tachycardia is an increased heart rate for any reason. If a fast heart rate is caused by exercise or stress, it's called sinus tachycardia. Sinus tachycardia is a symptom, not a condition.
Most heart conditions can lead to different forms of tachycardia. Irregular heart rhythms, called arrhythmias, are one cause. An example of an irregular heart rhythm is atrial fibrillation (AFib).
Other things that may lead to tachycardia include:
- Fever.
- Excessive alcohol use, which is defined as 14 or more drinks a week for a man or seven or more drinks a week for a woman.
- Alcohol withdrawal.
- Too much caffeine.
- High or low blood pressure.
- Changes in the level of minerals in the body, called electrolytes. Examples include potassium, sodium, calcium and magnesium.
- Certain medicines.
- Overactive thyroid, called hyperthyroidism.
- A low number of red blood cells, called anemia.
- Smoking or nicotine use.
- Use of illegal stimulants such as cocaine or methamphetamine.
- Heart attack.
Sometimes the exact cause of tachycardia is not known.
How does the heart beat?
Typical heartbeat
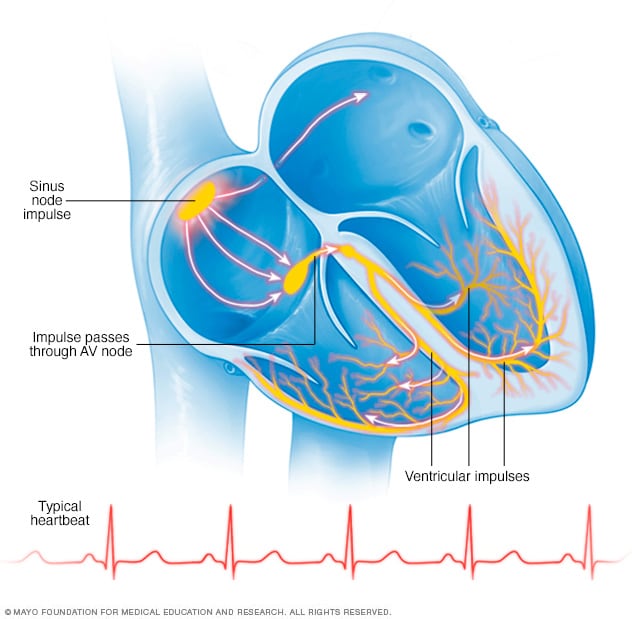
Typical heartbeat
In a typical heart rhythm, a tiny cluster of cells at the sinus node sends out an electrical signal. The signal then travels through the atria to the atrioventricular (AV) node and then passes into the ventricles, causing them to contract and pump out blood.
To understand the cause of tachycardia, it may be helpful to know how the heart usually works.
The heart has four chambers:
- The two upper chambers are called the atria.
- The two lower chambers are called the ventricles.
Inside the upper right heart chamber is a group of cells called the sinus node. The sinus node makes the signals that start each heartbeat.
The signals move across the upper heart chambers. Then the signals arrive at a group of cells called the AV node, where they usually slow down. The signals then go to the lower heart chambers.
In a healthy heart, this signaling process usually goes smoothly. The resting heart rate is typically 60 to 100 beats a minute. But in tachycardia, something causes the heart to beat faster than 100 beats a minute.
Risk factors
In general, things that may raise the risk of irregular heart rhythms that commonly cause tachycardia include:
- Getting older.
- Having a family history of some heart rhythm disorders.
- High blood pressure.
Lifestyle changes or treatment of heart conditions may lower the risk of tachycardia.
Complications
When the heart beats too fast, it may not pump enough blood to the body. As a result, the organs and tissues may not get enough oxygen.
Complications of tachycardia depend on:
- The type of tachycardia.
- How fast the heart is beating.
- How long the rapid heart rate lasts.
- Whether there are other heart conditions.
Potential complications of tachycardia may include:
- Blood clots that can cause a heart attack or stroke. Blood-thinning medicine may be used to lower this risk.
- Frequent fainting or unconsciousness.
- Heart failure.
- Sudden cardiac death. This is usually only associated with ventricular tachycardia or ventricular fibrillation.
Prevention
The best way to prevent tachycardia is to keep the heart healthy. Have regular health checkups. If you have heart disease, follow your treatment plan. Take all medicines as directed.
Try these tips to prevent heart disease and keep the heart healthy:
- Don't smoke.
- Eat a diet that's low in salt and saturated fat.
- Exercise at least 30 minutes a day on most days of the week.
- Maintain a healthy weight.
- Reduce and manage stress.
- Control high blood pressure, high cholesterol and diabetes.
- Get good sleep. Adults should aim for 7 to 9 hours daily.
Talk to your healthcare team before using any medicines. Some cold and cough medicines have stimulants that may start a rapid heartbeat. Illegal drugs such as cocaine and methamphetamine are other stimulants that can cause changes in the heart's rhythm.
Dec. 15, 2023